End stage alcoholism is the most serious phase of alcohol addiction, marked by severe health issues and a high risk of death. This article will outline what defines end stage alcoholism, its symptoms, health risks, and treatment options. We’ll also provide guidance on supporting a loved one who is affected.
Key Takeaways
- End stage alcoholism is characterized by irreversible organ damage, severe cognitive decline, and a significantly reduced life expectancy, generally leading to life-threatening health complications.
- Key signs of end stage alcoholism include severe withdrawal symptoms, cognitive impairments such as memory loss, and behavioral changes like social withdrawal and neglect of personal hygiene.
- Treatment is possible through medically supervised detox and long-term care, but recovery requires a commitment to sobriety and ongoing medical support to manage the severe consequences of alcohol dependence.
What is end stage alcoholism?
End stage alcoholism is the terminal phase of alcohol addiction, marked by organ failure, cognitive decline, and often a high risk of death without intervention. This stage develops after prolonged alcohol consumption, leading to critical health and psychological issues that severely impair daily functioning. Individuals suffering from end stage alcoholism and severe alcohol use disorder often face significant organ damage, severe social ramifications such as job loss and isolation, and a considerable reduction in life expectancy. In the end stages of severe alcohol use disorder, these challenges become even more pronounced, particularly for those with alcohol misuse and alcohol use disorder AUD.
Without intervention, this phase can lead to life-threatening consequences, including death. Severe health complications such as liver disease, heart problems, and cognitive impairments are common, making this stage the most critical and severe form of alcohol dependence. Individuals may experience severe withdrawal symptoms when not consuming alcohol, further complicating their condition.
How does end stage alcoholism differ from earlier stages?
Early-stage alcoholism is driven by increasing alcohol tolerance, where individuals may still engage in social drinking and maintain some control over their drinking behaviors. As alcoholism progresses to the middle stage alcoholism, physical dependence becomes more apparent, and the person may experience withdrawal symptoms if they stop drinking. Health issues may begin to emerge in these early stages, but they are often not as severe or life-threatening as those in end stage alcoholism.
End stage alcoholism is characterized by irreversible organ damage and severe alcohol dependency. Individuals face life-threatening health issues such as liver failure and severe neurological damage, which are rare in earlier stages. Late stage alcohol addiction leads to significant social interactions diminishing, resulting in marked isolation and withdrawal from loved ones. Alcohol addiction is a serious concern that compounds these issues.
Cognitive impairments like severe memory lapses and decision-making difficulties become much more pronounced, severely affecting daily life consequences.
Signs and symptoms of end stage alcoholism
End stage alcoholism presents a multitude of signs and symptoms that impact physical health, cognitive function, and social behavior. The physical toll includes severe withdrawal symptoms, liver failure, and significant weight loss. Cognitive decline includes memory loss, confusion, and psychiatric disturbances, while social and behavioral signs include isolation, neglect of personal hygiene, and erratic behavior.

Physical symptoms
Individuals in the final stage of alcoholism may experience:
- Severe weight loss due to nutritional deficiencies and metabolic changes
- Jaundice, a yellowing of the skin and eyes indicative of liver failure
- Chronic tremors
- Pronounced gastrointestinal issues
- Frequent infections due to a weakened immune system
Fluid retention, resulting in swelling in the legs and abdomen, along with severe fatigue and weakness, are common physical symptoms.
Cognitive and mental health decline
Cognitive functions often deteriorate significantly in end stage alcoholism, leading to disorientation, confusion, and severe memory lapses. Individuals may experience emotional instability, with marked mood swings and increased irritability, particularly when alcohol is unavailable — symptoms that can indicate the early onset of alcoholic dementia.
Social withdrawal and isolation are common, driven by shame and stigma associated with their addiction.
Social and behavioral signs
Behavioral changes in end stage alcoholism include:
- Increased irritability and mood swings
- Withdrawal from social interactions
- Neglect of personal hygiene
- Erratic or aggressive behavior
These behaviors reflect the severe impact of heavy drinking on a person’s social life and overall behavior.
Health complications caused by end stage alcoholism
End stage alcoholism results in significant damage to vital organs, leading to severe health complications. These include:
- Liver diseases
- Cardiovascular issues
- Neurological damage
- Pancreatitis
The severity of these complications underscores the risks of life threatening complications associated with prolonged alcohol abuse and excessive alcohol use, as well as the urgency of addressing this condition.

Liver diseases
Liver damage in the final stages of alcoholism can lead to cirrhosis and fatty liver disease. Cirrhosis, characterized by severe scarring and liver dysfunction, is the most severe and often irreversible stage of liver disease, frequently requiring a liver transplant. Complications from cirrhosis can lead to life-threatening situations like ascites and variceal bleeding.
Symptoms of alcoholic liver disease may initially go unnoticed but can eventually manifest as digestive problems, jaundice, and memory issues.
Cardiovascular issues
Chronic alcohol abuse increases the likelihood of heart disease and elevates the risk of stroke. Conditions like cardiomyopathy, which affects the heart muscle, become more pronounced in the final stages, significantly impacting cardiovascular health.
These severe health complications underscore the critical nature of severe alcohol end stage alcoholism on the cardiovascular system, which can lead to serious health problems.
Neurological damage
End stage alcoholism can cause cognitive impairments and conditions like Wernicke-Korsakoff Syndrome due to vitamin deficiencies. This syndrome, associated with heavy alcohol use, leads to severe memory disorders. Long-term alcohol abuse also results in alcoholic neuropathy, causing nerve damage primarily affecting the legs and feet.
The neurological effects range from mild cognitive disturbances to serious conditions requiring long-term care.
Pancreatitis and gastrointestinal damage
Long-term alcohol consumption can cause pancreatitis, characterized by inflammation of the pancreas and severe abdominal pain. Chronic alcohol consumption causes a significant percentage of acute pancreatitis cases, with recurrent attacks often leading to chronic pancreatitis.
Patients with alcohol-related pancreatitis may experience significant abdominal pain and other gastrointestinal symptoms such as nausea and anorexia.
How long can you live with end stage alcoholism?
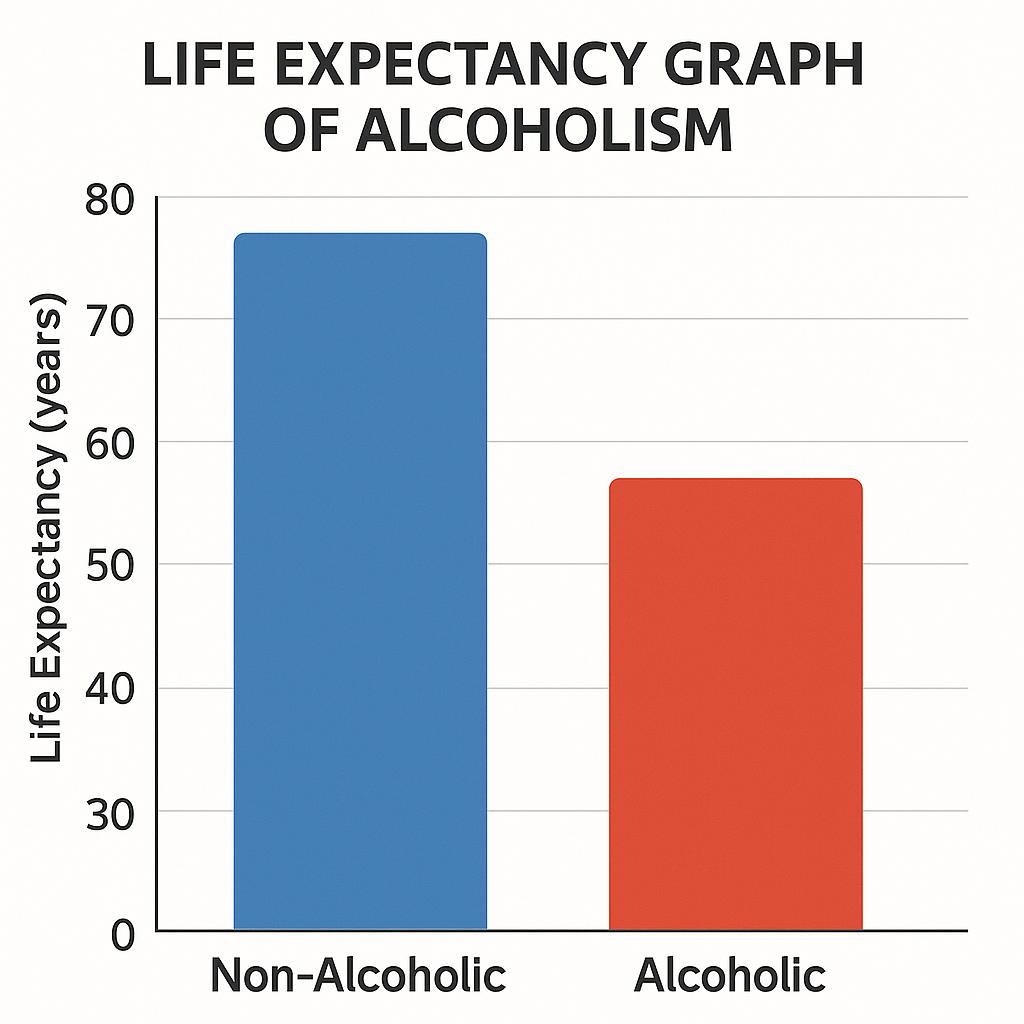
Individuals with end stage alcoholism typically have a reduced lifespan of around 30 years due to complications from alcohol-related diseases. Life expectancy varies based on the extent of organ damage and whether the individual accepts treatment. For example, patients with decompensated cirrhosis from alcohol have a 5-year survival rate of around 20%, illustrating the severe impact of liver-related complications.
Timely medical intervention and lifestyle changes can improve a person’s life and survival rates. The journey towards recovery, while challenging, can extend life expectancy if managed properly, as shown in a structured alcohol recovery timeline. Seeking medical help and making necessary changes can halt disease control progression.
Can end stage alcoholism be treated?
Treatment options for end stage alcoholism are available, though their effectiveness varies depending on individual circumstances. Medically supervised detox reduces withdrawal risks, and in some cases, alcohol addiction medication may also be used to support long-term recovery, while long-term care or hospice provides comfort and support.
Liver transplant eligibility and recovery depend on factors like the patient’s commitment to sobriety and overall health.
Detox and medical stabilization
Detoxification from alcohol is often the first step in treatment, focusing on managing alcohol withdrawal symptoms and ensuring medical safety. Medical detox is critical for managing withdrawal symptoms safely, especially for those with advanced alcoholism, as unsupervised withdrawal can be fatal.
A supervised detox program enhances comfort and safety, significantly aiding those in late stages of alcoholism in achieving sobriety and helping them avoid withdrawal symptoms.
Long-term care and hospice
Long-term care may involve supportive services and hospice care for those in the final stages, aiming to improve their quality of life. Hospice care focuses on:
- Comfort and symptom management rather than curative treatment
- Pain management
- Psychological support
- Family involvement, which is crucial for emotional support
Liver transplant considerations
A liver transplant can be viable for patients with end stage alcoholism but typically requires a period of sobriety before eligibility. The criteria for liver transplantation include the recognition of alcoholism, psychiatric stability, and the presence of supportive relationships.
Evidence suggests that selected alcoholic patients can survive liver transplants and reintegrate into society, challenging the notion that they are less deserving.
What to do if your loved one is in the end stage of alcoholism
Intervention at the end stage of alcoholism is crucial to address severe medical and mental health problems. Support from addiction specialists, mental health professionals, and family is vital in overcoming alcoholism and managing this condition, as highlighted by the mental health services administration.
Caregivers should prepare for resistance and ensure the safety and well-being of their loved one by seeking professional help, joining support groups, and creating a supportive environment.

Emergency signs to watch for
Signs indicating a medical emergency for someone in end stage alcoholism include:
- Confusion
- Severe agitation
- Unresponsiveness
- Seizures
- Severe tremors
- Hallucinations
- Uncontrolled vomiting, especially if blood is present
- Severe dehydration or malnutrition
These symptoms require immediate medical attention.
When to consider hospice or inpatient treatment
Consider inpatient treatment or hospice care when a loved one has significant health complications and a poor prognosis. Hospice care is appropriate when a patient’s life expectancy is limited to six months or less due to advanced alcoholism. Signs indicating the need for hospice include significant weight loss, recurrent infections, and the inability to perform daily activities.
Family involvement is crucial in deciding on hospice care.
How is end stage alcoholism diagnosed?
Diagnosing end stage alcoholism involves:
- Clinical history: assessing the patient’s history of alcohol consumption.
- Physical signs: identifying severe health deterioration such as jaundice or ascites.
- Liver function tests: evaluating the extent of liver damage.
- Cognitive assessments: evaluating cognitive impairments.
Physical examinations often reveal critical indicators of advanced liver disease. Withdrawal symptoms or other psychological conditions may also be considered during diagnosis.
Overall, a comprehensive diagnostic approach is essential for accurately identifying and managing end stage alcoholism.
Is recovery from end stage alcoholism ever possible?
While end stage alcoholism suggests imminent death, recovery is still feasible with appropriate medical support and intervention. Detoxification helps manage dangerous withdrawal symptoms, making it critical for recovery. Inpatient rehabilitation is recommended for those in advanced stages to enhance the chances of maintaining sobriety and avoiding alcohol relapse.
Medical assistance during detox ensures safety and comfort. Although recovery from late-stage alcoholism can extend life expectancy if managed properly, it requires a strong commitment to sobriety and continuous medical support.
Resources for support and next steps
Numerous resources are available to support and guide those dealing with end stage alcoholism. The SAMHSA National Helpline offers confidential and free help for individuals and families facing substance abuse issues. The National Institute on Alcohol Treatment Navigator helps you find alcohol rehab options in your area. The National Institute on alcohol abuse also provides valuable information and resources for those seeking assistance.
Local detox and rehab centers provide essential services for managing severe withdrawal and starting recovery. Additionally, addiction medicine providers and programs like Firepit Health offer telehealth-based support for late-stage cases, ensuring that help is accessible regardless of location.
Bottom Line: End Stage Alcoholism
The end stage of alcoholism is the most critical phase of alcohol use disorder, marked by severe health complications, significant cognitive decline, and a drastically reduced life expectancy. Recognizing the signs and symptoms, understanding the health complications, and knowing the treatment options are crucial steps in managing this condition. Support from healthcare professionals, addiction specialists, and family is vital in navigating this challenging journey.
Although the road to recovery from end-stage alcoholism is arduous and fraught with challenges, it is not entirely without hope. By seeking timely medical intervention and leveraging available resources, individuals and their loved ones can strive for a better quality of life. Remember, every step taken towards understanding and managing this condition is a step towards overcoming the devastating effects of alcoholism.
FAQs about end-stage alcoholism
Can someone survive end-stage alcoholism?
Survival is possible but extremely challenging for those in end-stage alcoholism. With medical intervention and significant lifestyle changes, some may extend their life expectancy, though the situation remains critical.
What are the final symptoms before death from alcoholism?
The final symptoms before death from alcoholism typically include severe liver failure, jaundice, and significant cognitive decline. These indications point to critical organ damage and a deteriorating condition.
Does hospice treat alcoholism?
Hospice does not treat alcoholism; instead, it focuses on providing comfort and managing symptoms to enhance quality of life in the final stages.
What happens to the brain in end stage alcoholism?
In end stage alcoholism, the brain experiences severe cognitive impairments and memory loss, often leading to conditions such as Wernicke-Korsakoff Syndrome. This deterioration significantly affects both mental and physical health.
What resources are available for support?
There are several valuable resources for support, including the SAMHSA National Helpline, the NIAAA Alcohol Treatment Navigator, local detox and rehab centers, and telehealth programs like Firepit Health. Utilizing these resources can provide necessary assistance and guidance.
















