How long does Suboxone stay in your system? Usually up to seven days, depending on the test and personal factors like metabolism and dosage. This article covers the detection windows across different tests and what influences these times.
Key Takeaways
- Suboxone can be detected in various drug tests for different durations, with urine tests detecting buprenorphine for up to 10 days and hair tests for up to 90 days.
- The half-life of Suboxone’s main component, buprenorphine, ranges from 24 to 48 hours, while its metabolite, norbuprenorphine, can remain for approximately 150 hours, affecting withdrawal and tapering processes.
- Detection times of Suboxone are influenced by individual factors such as metabolism, liver function, and dosage, highlighting the need for personalized treatment plans.
How long does Suboxone stay in your system? Quick facts
In general, Suboxone can remain detectable in your system for up to seven days. Key points about its components include:
- The half-life of buprenorphine, the primary component, ranges between 24 to 42 hours.
- Naloxone has a shorter half-life of 2 to 12 hours.
- Buprenorphine stays in your system longer, contributing to the extended detection times.
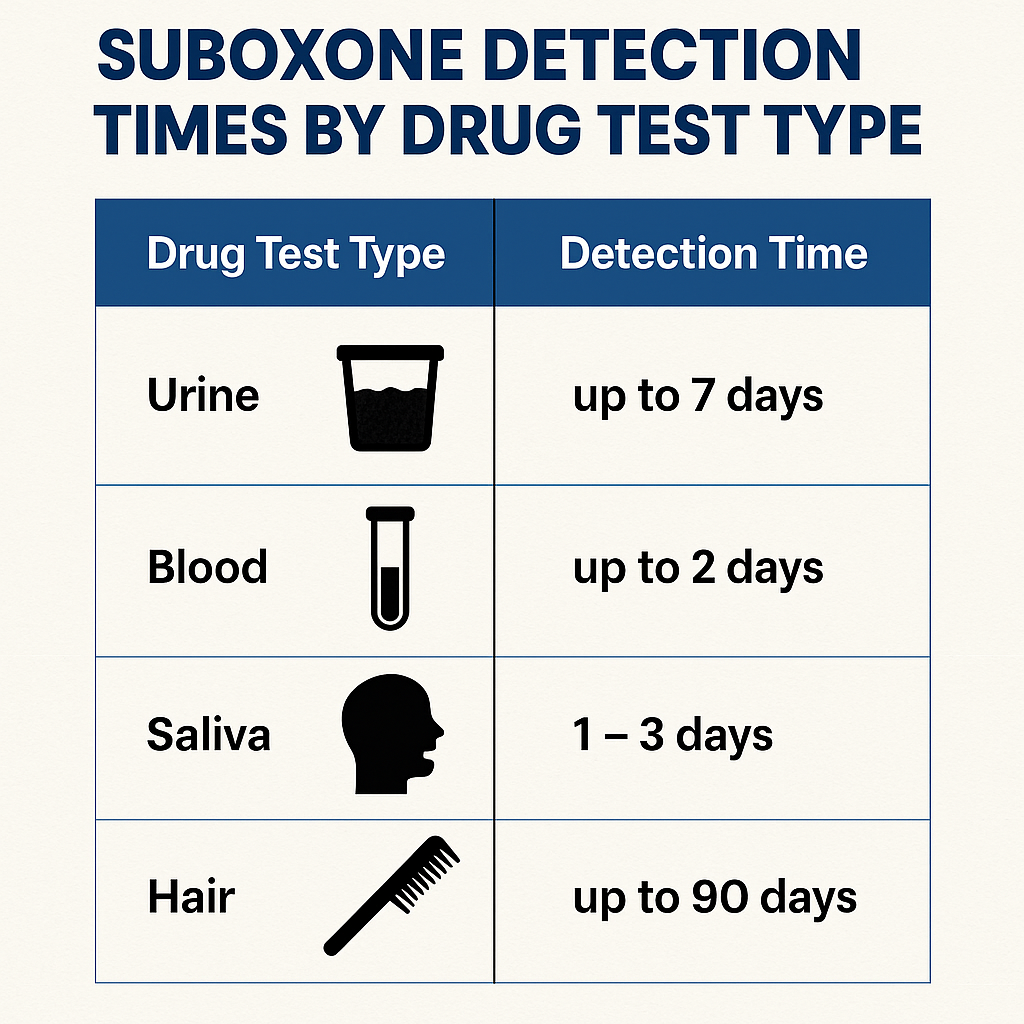
Suboxone can be detected in drug tests for different lengths of time. Each type of drug test has its own detection window for this substance:
- Urine tests, the most common type, can detect buprenorphine for up to a week.
- Blood tests generally detect Suboxone for 1 to 2 days after the last dose.
- Saliva tests offer a detection window of about 2 to 3 days.
- Hair tests can reveal Suboxone use for up to 90 days.
These windows are influenced by several factors influencing, including the dosage, metabolism, frequency of drug use, and euphoric effects of drugs, as well as varying detection windows. This is where the term drug refers to the various substances involved.
Understanding that Suboxone contains both buprenorphine and naloxone, each with different durations in the body, aids in planning treatment, avoiding interactions, and managing the withdrawal process.
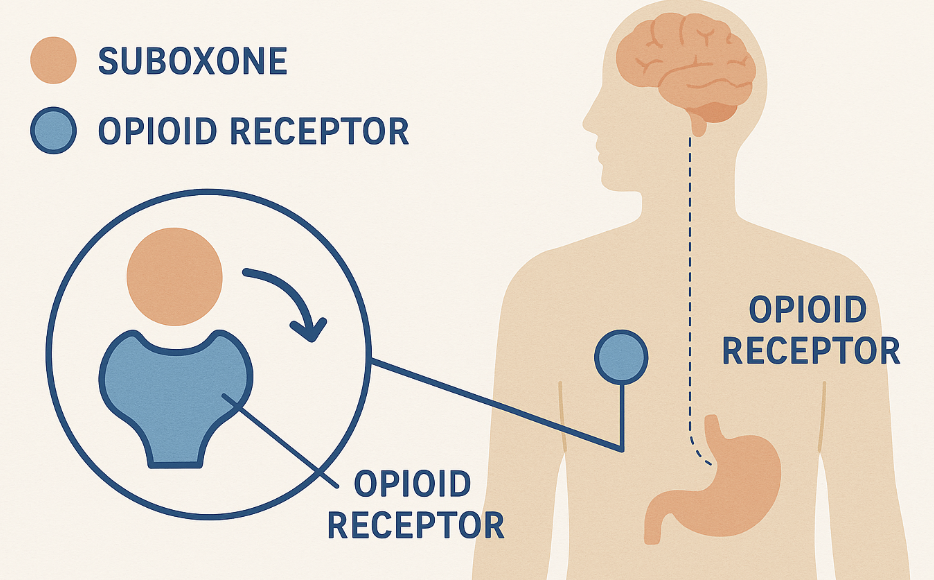
What is Suboxone, and how does it work?
Suboxone is a prescription medication that requires a prescription as it is classified as a controlled substance. It is used to treat opioid addiction. It combines buprenorphine, a partial opioid agonist, and naloxone, an opioid antagonist. Buprenorphine helps alleviate withdrawal symptoms and cravings without causing significant intoxication, which addresses common questions about whether Suboxone gets you high. Naloxone, on the other hand, is included to deter misuse; it can induce withdrawal symptoms if the drug is taken through non-prescribed routes like injection. Suboxone block opioids.
Suboxone is highly suboxone effective in medication-assisted treatment (MAT) programs for opioid use disorder (OUD) and is a crucial component in treating opioid addiction. Key points about starting Suboxone treatment include:
- Patients are usually required to abstain from opioids for 12-24 hours before starting treatment.
- This initial abstinence helps ease the transition to Suboxone.
- It minimizes the risk of precipitated withdrawal symptoms when starting the medication.
The use of Suboxone in a comprehensive treatment plan often includes psychosocial support, such as group therapy and counseling. This holistic approach enhances recovery outcomes, providing a stable foundation for long-term sobriety and reducing the risk of relapse in addiction treatment.
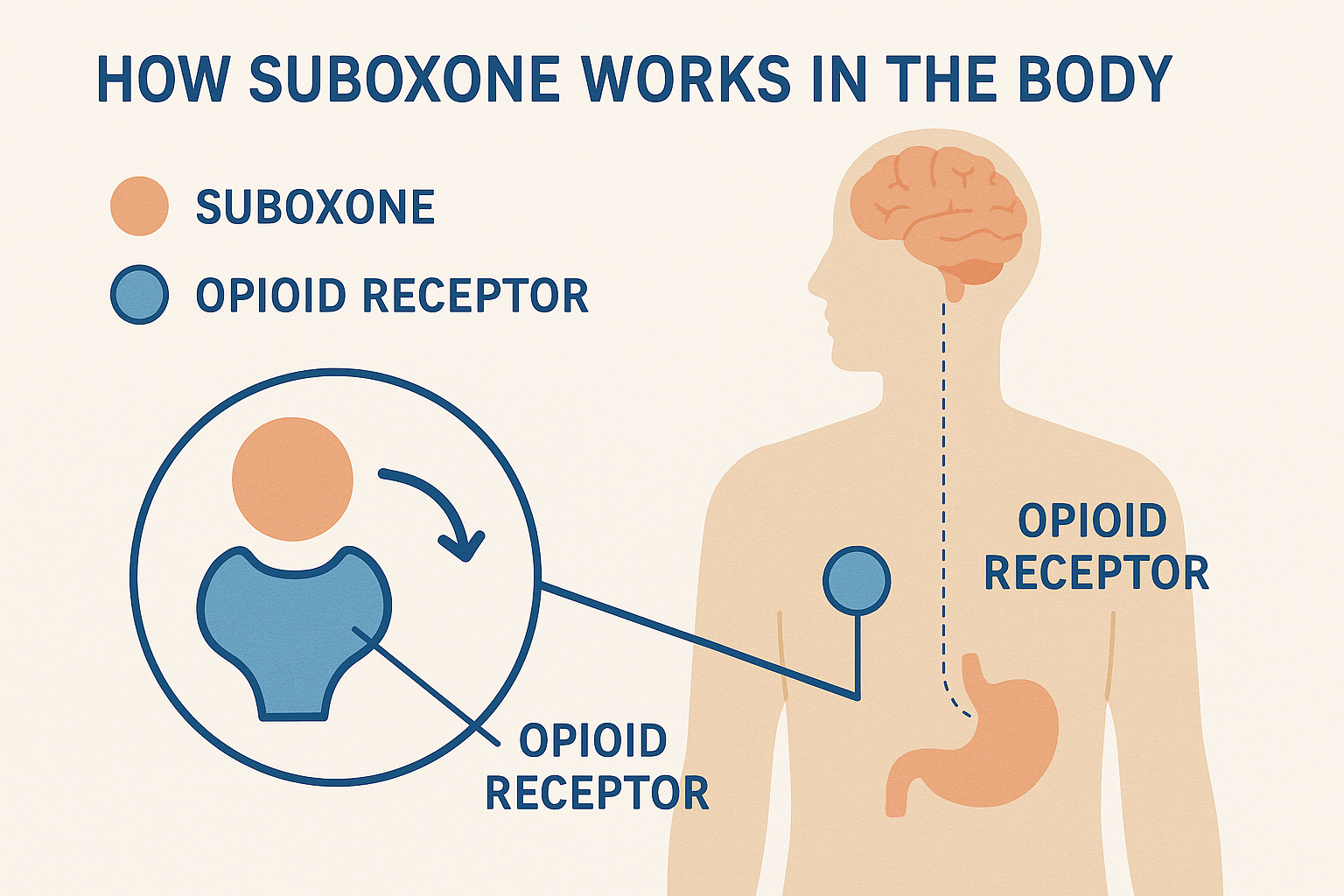
How Suboxone is metabolized in the body
Suboxone is typically administered sublingually, meaning it is placed under the tongue to dissolve. This method allows the medication to be absorbed directly into the bloodstream, reaching peak levels within 1 to 4 hours. Once absorbed, buprenorphine is metabolized primarily by the liver through the CYP3A4 pathway, converting into norbuprenorphine, a metabolite that remains in the system longer.
The half-life of buprenorphine ranges from 24 to 48 hours, while norbuprenorphine has a significantly longer half-life of about 150 hours. This extended presence in the body means that Suboxone can be detected for up to 14 days after use, largely due to the prolonged presence of its metabolite. Factors such as body composition, age, and overall liver health significantly influence how quickly Suboxone is metabolized.
Naloxone, the other component of Suboxone, has limited bioavailability when taken sublingually and a short half-life when active, usually around 30 to 90 minutes. This short duration of action is sufficient to deter misuse without significantly contributing to the overall detection window of Suboxone.
Suboxone detection times by drug test type
Urine tests are widely used to detect Suboxone use. They are one of the most common testing methods available. In urine, buprenorphine can be detected for up to 7 to 10 days, while naloxone is usually present for a shorter period. Blood tests offer a more limited detection window, typically identifying Suboxone use within 24 to 72 hours after the last dose.
Saliva tests are another option, with buprenorphine detectable for about 2 to 3 days. Hair tests, however, provide the longest detection window, capable of revealing Suboxone use for up to 90 days.
Many standard opioid panels do not detect Suboxone unless buprenorphine-specific testing is used. Knowing these detection windows helps patients and healthcare providers manage treatment plans more effectively and ensure compliance with medication-assisted treatment programs.
Factors that affect how long Suboxone stays in your system
Several factors influence how long Suboxone stays in your system, and these can vary from person to person. Dosage and duration of use are primary factors; chronic use results in longer detection times compared to a one-time dose. Metabolism and liver function are also crucial, as the liver metabolizes buprenorphine into norbuprenorphine.
Factors that impact the rate at which Suboxone is processed and eliminated from the body include:
- Age
- Weight
- Body fat percentage
- Overall health
- Concurrent medications, especially those affecting the CYP3A4 enzyme, can alter the metabolism of Suboxone, so it's important to understand what medications you should not take with Suboxone.
Additionally, hydration levels and kidney function influence the speed at which Suboxone is excreted from the body. These factors highlight the variability in Suboxone detection times and underscore the importance of personalized treatment plans tailored to individual needs.
Why knowing how long Suboxone stays in your system matters
Understanding how long Suboxone stays in your system is crucial for several reasons. For one, it helps avoid interactions with other opioids, which can lead to precipitated withdrawal. Knowing the duration also aids in preparing for detox or tapering off the medication, ensuring a smoother transition and minimizing withdrawal symptoms.
Compliance with medication-assisted treatment programs is another significant aspect. Accurate knowledge of Suboxone’s presence helps healthcare providers manage treatment effectively and supports patients in adhering to their prescribed regimen, especially in the context of preventing drug abuse.
Finally, understanding the timeline of opioid withdrawal symptoms can help patients and providers anticipate and manage discomfort to ease withdrawal symptoms after the last dose.

How Suboxone's half-life affects withdrawal and tapering
The half-life of Suboxone significantly impacts the withdrawal process and the tapering schedule. With a half-life ranging from 24 to 48 hours, Suboxone withdrawal symptoms typically peak within the first 72 hours and can last up to a month. This extended duration necessitates a carefully managed tapering process to minimize discomfort.
A longer half-life allows for a smoother tapering process, reducing the severity of Suboxone withdrawal symptoms experienced by the user. Medical supervision during tapering is essential due to the delayed onset of symptoms, ensuring that adjustments to the tapering schedule can be made as needed.
Options for managing withdrawal include microdosing or transitioning to alternatives like Sublocade or Brixadi, which may offer more controlled dosing and symptom management. These treatment options and other medications help ease the transition and support long-term recovery efforts.
Does anything make Suboxone leave your system faster?
No safe method exists to rapidly “flush” Suboxone from your system. Various detox myths and unproven remedies often lack scientific backing and can be dangerous. Speeding up the elimination process without medical guidance can lead to severe complications.
Medical supervision during tapering is the safest and most effective approach to managing Suboxone use, especially when done through a Suboxone detox program. Healthcare providers can create a tailored plan that gradually reduces the dosage, minimizing common suboxone withdrawal symptoms and ensuring a safer transition off the medication.
How long does Suboxone stay in your system vs. other opioids?
Suboxone remains in the body longer than many other opioids due to its long elimination half life of 24 to 48 hours. For example, methadone has a half-life of 8 to 59 hours, while naloxone remains active for only 30 to 90 minutes. This extended duration makes Suboxone particularly effective in preventing relapse and managing withdrawal symptoms over a more extended period, as the drug’s half life contributes to its effectiveness.
In contrast, opioids like heroin and morphine typically have shorter detection windows, which can lead to frequent dosing and a higher risk of relapse. Suboxone’s longer-acting coverage provides a significant advantage in maintaining sobriety and supporting long-term recovery efforts with full opioid agonists, opioid antagonists, drug addiction, and opioid addiction treatment.
What to do if you’re concerned about Suboxone in your system
If you’re concerned about clear suboxone in your system, the first step is to consult your healthcare provider before taking suboxone or making any changes to your suboxone dose. Abruptly stopping or altering your medication can lead to severe withdrawal symptoms and other health risks.
Medication-assisted treatment (MAT) programs and telehealth services offer support and guidance for managing Suboxone use and withdrawal. These programs provide a structured approach to tapering and ensure that you receive the necessary medical supervision to safely transition off the medication.
Bottom Line: How long does Suboxone stay in your system
Suboxone can remain detectable in your body for up to a week, with specific detection windows varying by test type:
- Urine tests can detect buprenorphine for up to 7 to 10 days
- Blood tests for 24 to 72 hours
- Saliva tests for 2 to 3 days
- Hair tests for up to 90 days
Individual factors such as metabolism, liver function, and dosage significantly influence these detection times.
Understanding Suboxone metabolism and suboxone detection windows is crucial for managing treatment, avoiding drug interactions, and preparing for withdrawal. This knowledge supports better treatment outcomes and helps patients maintain compliance with their recovery programs.
FAQs About How long does Suboxone stay in your system
How long does Suboxone stay detectable in urine?
Suboxone remains detectable in urine for approximately 7 to 10 days following the last administration. This timeframe is essential for understanding its potential presence in drug testing scenarios.
Does Suboxone show up on standard drug tests?
Suboxone typically does not appear on standard drug tests unless a specific test for buprenorphine is administered. Therefore, if you are concerned about detection, it is advisable to clarify which type of drug test will be used.
What factors influence how long Suboxone stays in your system?
The duration Suboxone remains in your system is primarily influenced by dosage, metabolism, liver function, age, weight, and any concurrent medications. These factors collectively determine the drug's elimination rate and overall presence in the body.
Are there any methods to quickly remove Suboxone from the body?
No safe methods exist to quickly remove Suboxone from your body; the safest option is to undergo medical supervision during tapering.
Why is it important to know how long Suboxone stays in your system?
Understanding the duration Suboxone remains in your system is crucial for preventing negative interactions with other opioids, effectively managing detox or tapering processes, and maintaining adherence to treatment protocols. This knowledge ensures a safer and more effective recovery journey.