If you’re considering Naltrexone vs Suboxone for addiction treatment, it’s important to understand how they differ. Naltrexone is an opioid antagonist that blocks opioid effects, suited for those fully detoxed. Suboxone reduces cravings and withdrawal symptoms, ideal for early-stage recovery. This article compares their uses, benefits, and drawbacks.
Key Takeaways
- Naltrexone is an opioid antagonist that blocks opioid receptors, making it effective for maintaining abstinence from opioids and alcohol, while Suboxone combines buprenorphine and naloxone to manage cravings and withdrawal symptoms.
- Naltrexone is non-addictive and requires patients to be opioid-free for 7-14 days before treatment, whereas Suboxone may lead to dependence and requires a tapering process upon discontinuation.
- Naltrexone is approved for alcohol use disorder, while Suboxone is strictly for opioid addiction, underscoring the need for careful consideration of individual treatment needs and co-occurring conditions.
What is the difference between Naltrexone and Suboxone?
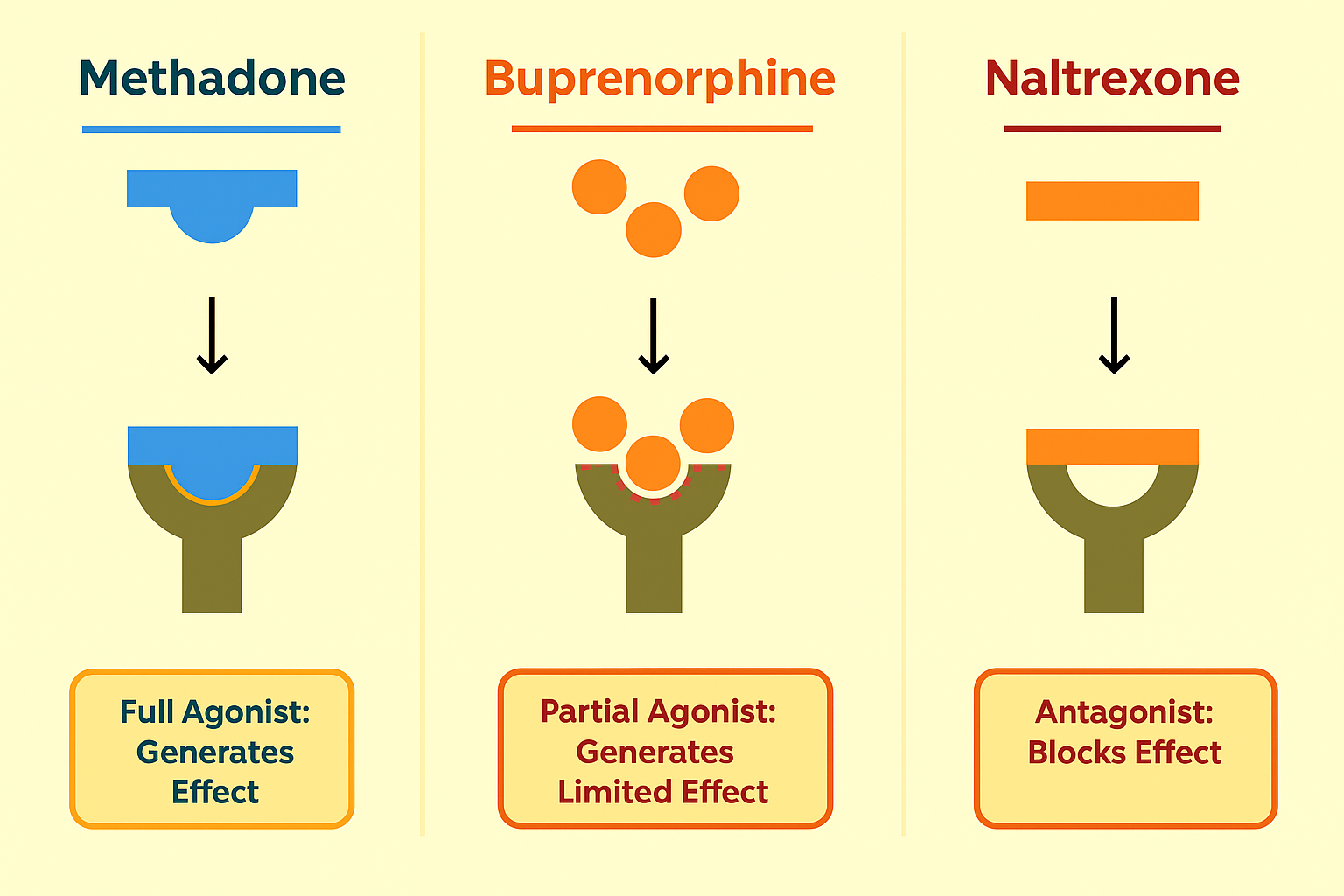
Naltrexone and Suboxone serve vital roles in addiction treatment, yet they operate through distinct mechanisms. Naltrexone is an opioid antagonist, which means it blocks opioid receptors in the brain, preventing the euphoric effects of opioids and alcohol. On the other hand, Suboxone combines buprenorphine, a partial opioid agonist, with naloxone to reduce cravings and withdrawal symptoms while lowering the risk of misuse. Both medications are approved for opioid addiction treatment, but only Naltrexone is approved for alcohol use disorder (AUD) as well.
Naltrexone is available in both pill form and as an extended-release monthly injection known as Vivitrol. This makes it a non-replacement therapy, as it does not substitute one opioid for another. Conversely, Suboxone is typically administered as a daily oral film or tablet and is used during the initial withdrawal phase to manage symptoms and cravings. Unlike methadone treatment, which can be highly addictive, Suboxone’s partial agonist properties offer a safer alternative while still providing relief from withdrawal.
Extended-release naltrexone is non-addictive and does not cause withdrawal symptoms upon cessation. However, it requires patients to be fully detoxed from opioids for 7-14 days before starting treatment to avoid severe opioid withdrawal symptoms.
Suboxone, while effective in reducing cravings, reduces cravings and carries the risk of drug dependence due to its buprenorphine content, necessitating a tapering process when stopping.
How does Naltrexone work?
Naltrexone functions as a pure opioid antagonist, meaning it naltrexone binds to opioid receptors in the brain’s opioid receptors and blocking opioid receptors without activating them. This action prevents the user from experiencing the pleasurable and sedative effects associated with opioids like heroin and morphine, thereby reducing cravings and helping maintain abstinence. Naltrexone is available in two forms: an oral pill (Revia) and an extended-release monthly injection (Vivitrol), offering flexibility in administration.
For Naltrexone to be effective, patients must undergo a complete detoxification process, remaining opioid-free for 7-10 days before starting the medication. Unlike methadone or buprenorphine treatment, which involve partial activation of opioid receptors to suppress cravings, Naltrexone strictly blocks these receptors, making it a non-addictive option.
However, patients should be aware that Naltrexone does not alleviate withdrawal symptoms and should be integrated into a comprehensive treatment plan that includes counseling and support programs.
How does Suboxone work?
Suboxone is a combination medication comprising buprenorphine and naloxone. Buprenorphine is a partial opioid agonist, which means it partially activates opioid receptors in the brain, reducing cravings and alleviating withdrawal symptoms without producing the full euphoric effects of opioids. This mechanism helps stabilize patients during the initial stages of recovery and supports long-term maintenance therapy.
Naloxone, the other component of buprenorphine naloxone, is an opioid antagonist included to deter misuse. If Suboxone is injected rather than taken as prescribed (sublingually or buccally), naloxone precipitates withdrawal symptoms, thereby discouraging abuse.
The medication is typically administered daily and is available in sublingual or buccal forms, offering flexibility in dosing. This dual-action approach makes Suboxone a valuable tool in both detoxification and long-term maintenance phases of opioid addiction treatment.
Naltrexone vs Suboxone: Benefits and drawbacks
Both Naltrexone and Suboxone play crucial roles in aiding individuals recovering from substance use disorders, but their distinct mechanisms and effects come with unique benefits and drawbacks.
A deeper dive into these aspects can help patients and healthcare providers make more informed decisions.
Benefits of Naltrexone
Naltrexone offers several key benefits in addiction treatment. One of its most significant advantages is its non-addictive nature; patients do not develop a dependence on the medication and, therefore, do not require tapering when discontinuing use. Additionally, the availability of a long-acting monthly injection (Vivitrol) provides a convenient and effective option for those looking to maintain abstinence without the daily hassle of taking a pill.
Naltrexone treatment is effective in treating both opioid and alcohol addiction. It can be particularly beneficial for individuals with co-occurring alcohol use disorder (AUD) and opioid use disorder (OUD), offering a comprehensive approach to addiction treatment. The monthly injectable form ensures consistent medication levels in the body, enhancing adherence and therapeutic outcomes.
Drawbacks of Naltrexone
Despite its benefits, Naltrexone does have some drawbacks:
- A significant limitation is the requirement for a full detox before initiating treatment.
- Patients must be opioid-free for several days to avoid triggering severe withdrawal symptoms.
- This prerequisite can be a barrier for many individuals seeking immediate relief from addiction.
Another drawback is the lower retention rate in treatment programs compared to medications like Suboxone that help alleviate cravings. The oral version of Naltrexone has particularly poor adherence rates, as patients may struggle to remember daily dosing. Consequently, the injectable form is often preferred, although it may not be suitable for everyone.
Benefits of Suboxone
Suboxone offers several advantages, particularly in its ability to reduce cravings and withdrawal symptoms, which are critical during the early stages of recovery. By partially activating opioid receptors, Suboxone helps manage withdrawal symptoms, making the transition from opioid dependence more manageable. This can lead to higher retention rates in recovery programs, as patients experience less discomfort and are more likely to stick with their treatment plans.
The flexibility of daily dosing with Suboxone also adds to its benefits. Patients can take it sublingually or buccally, and the inclusion of naloxone reduces the risk of misuse. This makes Suboxone a versatile option for both detoxification and long-term maintenance therapy.
Drawbacks of Suboxone
However, Suboxone is not without its drawbacks. One of the main concerns is its potential for misuse if injected, despite the inclusion of naloxone to deter this behavior. Additionally, patients may develop physical dependence on suboxone addiction, necessitating a careful tapering process when discontinuing the medication.
Suboxone is not approved for treating alcohol addiction, limiting its use to opioid addiction only. For patients with a history of alcohol dependence, other treatment options must be considered. Moreover, the risk of developing psychological dependence and the need for long-term management can complicate treatment plans.
Who is Naltrexone best for?
Naltrexone is best suited for individuals who:
- Have fully detoxed from opioids and are committed to maintaining abstinence.
- Seek a non-addictive medication that does not carry the risk of dependence.
- Have co-occurring alcohol and opioid use disorders, as Naltrexone is effective in treating both conditions.
Additionally, Naltrexone is a good choice for individuals who prefer the convenience of a once-a-month injection over daily medication. This can be particularly beneficial for those with busy lifestyles or who have difficulty adhering to daily medication regimens. The monthly injection ensures consistent medication levels, improving adherence and treatment outcomes.
Who is Suboxone best for?
Suboxone is best suited for:
- Patients in the early stages of opioid recovery need immediate relief from withdrawal symptoms.
- Individuals who require the reduction of cravings and the management of withdrawal symptoms during the detoxification process.
- Those with a high risk of relapse.
- Individuals who experience intense cravings.
Patients engaged in structured Medication-Assisted Treatment (MAT) programs can greatly benefit from Suboxone, as it supports long-term opioid maintenance treatment therapy. The daily dosing regimen provides flexibility, allowing patients to take control of their recovery while reducing the risk of misuse through the inclusion of naloxone.
Naltrexone vs Suboxone for opioid use disorder
Both Naltrexone and Suboxone are effective in managing opioid use disorder (OUD), but they work through different mechanisms and are suited for different stages of recovery. Naltrexone, an opioid antagonist, blocks opioid receptors and prevents the euphoric effects of opioids, making it suitable for individuals who have already detoxed. Suboxone, combining buprenorphine (a partial agonist) and naloxone, helps reduce cravings and manage withdrawal symptoms, making it ideal for use during suboxone detox and the early stages of recovery.
Relapse risk and overdose prevention are critical considerations when choosing between these medications. Naltrexone is particularly effective in preventing relapse after detoxification, as it blocks the effects of opioids. However, patients must be aware of their diminished tolerance to opioids, as relapsing while on Naltrexone can lead to overdose. Suboxone, on the other hand, helps stabilize patients during recovery, reducing the risk of relapse by managing cravings and withdrawal symptoms.
Both medications require clinical supervision and ongoing monitoring to ensure safety and effectiveness. The comparison between vivitrol and suboxone shows how Naltrexone’s monthly injection offers consistent medication levels, while Suboxone’s daily dosing supports flexible detox support.

Naltrexone vs Suboxone for alcohol use disorder
When it comes to treating alcohol use disorder (AUD), Naltrexone is the clear choice. It is the only medication among the two that is FDA-approved for AUD, making it a reliable option for individuals seeking treatment for alcohol dependence. Naltrexone works by blocking the euphoric effects of alcohol, reducing cravings, and helping maintain abstinence.
Suboxone is not approved for treating alcohol use disorder and is not used for this purpose. Clinical studies have shown that Naltrexone is effective in reducing heavy drinking days and increasing the number of abstinent days in individuals with alcohol use disorders.
Supervised care is essential in the treatment of AUD, ensuring that patients receive comprehensive support and monitoring throughout their recovery journey.
Side effects and safety of Naltrexone vs Suboxone
Both Naltrexone and Suboxone have side effects and safety considerations that patients and healthcare providers must be aware of. Regular monitoring is essential, especially considering the potential liver-related complications associated with both medications.
Common side effects of Naltrexone
Common side effects of Naltrexone include:
- Nausea
- Headache
- Insomnia
- Fatigue
There is also a risk of liver disease and damage, which requires regular monitoring to ensure liver function remains within safe limits.
Patients should report any unusual symptoms to their healthcare provider promptly to manage these side effects effectively.
Common side effects of Suboxone
Some of the side effects of suboxone include constipation, dizziness, and sedation. Patients may also experience withdrawal symptoms if they abruptly stop taking the medication. In rare cases, Suboxone can lead to respiratory depression, particularly if taken in larger doses or combined with other depressants.
Anxiety and depression are also reported by some users.
Which medication is more effective?
The effectiveness of Naltrexone and Suboxone in treating opioid addiction can vary based on individual circumstances. Research indicates that both medications are effective, but their mechanisms and intended use differ. Naltrexone is primarily used to prevent relapse after detoxification, while Suboxone is aimed at managing withdrawal symptoms during recovery.
Factors influencing the effectiveness of these medications include the severity of the addiction, co-occurring conditions, and individual treatment goals. Combining medication with behavioral therapies has been shown to enhance the effectiveness of both Naltrexone and Suboxone in addiction treatment. Consulting with a healthcare provider can help determine the most appropriate medication based on these factors.
Can you switch from Suboxone to Naltrexone (or vice versa)?
Switching from Suboxone to Naltrexone (or vice versa) requires careful medical supervision to avoid complications such as precipitated withdrawal. Transitioning to Naltrexone necessitates a complete detoxification from opioids, which can take 7-14 days. During this period, patients should be monitored closely to manage any withdrawal symptoms.
Conversely, switching from Naltrexone to Suboxone is generally more straightforward but still requires medical oversight. A healthcare provider can help tailor the tapering process to minimize withdrawal symptoms and ensure a smooth transition.
It is crucial to follow medical advice closely during these transitions to maintain safety and treatment efficacy.
Factors to consider when choosing between Naltrexone and Suboxone
Several factors should be considered when choosing between Naltrexone and Suboxone. These include:
- The current status of substance use
- Whether the individual has completed detoxification
- The severity of cravings
- The risk of relapse, as Suboxone is more effective in managing these symptoms during the early stages of recovery.
Personal preferences, such as the choice between a daily oral medication and a monthly injection, play a role in determining the best treatment option. Co-occurring alcohol use or liver issues may influence the choice, as Naltrexone is effective for both alcohol and opioid addiction, but requires liver function monitoring.
The availability of medical monitoring and support is essential for the safe administration of both medications.
Other treatment options besides Naltrexone and Suboxone
Aside from Naltrexone and Suboxone, other opioid treatment options include Methadone, a full opioid agonist and one of the opioid agonists that has been used for decades in opioid addiction treatment. Methadone is effective in reducing cravings and withdrawal symptoms but carries a higher risk of dependence and requires strict medical supervision. This highlights the importance of a comprehensive treatment for opioid use disorder, medication strategies to treat opioid dependence, and to treat opioid medication.
Behavioral therapy and counseling are critical components of a comprehensive drug addiction treatment plan. These therapies can address the underlying psychological factors contributing to addiction and support long-term recovery.
Holistic and lifestyle-based support, such as exercise, nutrition, and mindfulness practices, can also play a significant role in maintaining sobriety and overall well-being.
Bottom Line: Naltrexone vs Suboxone, which one is right for you?
Naltrexone and Suboxone each have unique benefits and drawbacks, making them suitable for different stages and aspects of recovery. Naltrexone is ideal for those who have completed detoxification and are looking for a non-addictive option, while Suboxone is beneficial during the early stages of recovery to manage withdrawal symptoms.
Personal health history, preferences, and potential side effects are crucial factors to consider. Consulting with a healthcare provider is essential to determine the most appropriate medication for your specific needs and goals, which may require a doctor’s prescription.
Both medications should be part of a comprehensive treatment program that includes counseling and support for the best outcomes.
FAQs About Naltrexone vs Suboxone
Is Naltrexone stronger than Suboxone?
Naltrexone is not stronger than Suboxone; they serve different purposes in treatment. While Naltrexone blocks opioid receptors, Suboxone partially activates them, depending on the individual's recovery stage and treatment requirements.
Can I take Naltrexone after using Suboxone?
You can take Naltrexone after using Suboxone, but it is essential to undergo a detoxification period to prevent precipitated withdrawal. This process should be managed under the supervision of a healthcare provider.
Which has fewer side effects: Suboxone or Naltrexone?
Naltrexone generally has fewer side effects, like nausea and dizziness,s compared to Suboxone, which can cause constipation and sedation. However, individual responses may vary.
Is Naltrexone safe for long-term use?
Naltrexone is deemed safe for long-term use, provided that liver function is consistently monitored. Regular check-ups will ensure its safety and effectiveness in treatment.
Can Naltrexone help with cravings like Suboxone?
Naltrexone is not as effective as Suboxone in alleviating cravings, as it primarily blocks the euphoric effects of opioids instead of partially activating opioid receptors. Therefore, for managing cravings, Suboxone may be a more suitable option.















