Sublocade is a prescription medication used to treat opioid addiction. It is a monthly injection that contains buprenorphine, which helps reduce cravings and withdrawal symptoms. Moreover, it blocks the effects of opioids, aiding individuals in their recovery journey. In this article, we will explore what Sublocade is, how it works, its benefits, and more.
Key Takeaways
- Sublocade is an FDA-approved injectable medication for opioid use disorder that provides a steady release of buprenorphine over 30 days, reducing cravings and withdrawal symptoms.
- Unlike Suboxone, which is taken daily, Sublocade’s monthly administration minimizes missed doses and the risk of misuse, making it a viable option for individuals struggling with adherence.
- Patients must be stabilized on oral buprenorphine for at least a week before transitioning to Sublocade, and the medication must be administered by a certified healthcare provider due to its controlled substance status.
What is Sublocade, and how does it work?
Sublocade is a prescription medication specifically designed to aid in the treatment of opioid addiction, offering steady buprenorphine delivery through a monthly injection. It contains buprenorphine, an opioid partial agonist, and is administered as a monthly injection. This innovative treatment option works by binding to opioid receptors in the brain, effectively blocking the effects of other opioids and reducing cravings and withdrawal symptoms. The way sublocade work is by providing a sustained release of medication that helps manage addiction.
Sublocade differs from daily medications by:
- Providing a continuous release of buprenorphine over 30 days
- Maintaining consistent blood levels, minimizing the risk of missed doses and potential relapse
- Offering the convenience of a monthly injection, which enhances treatment adherence
This makes it a practical solution for individuals committed to overcoming opioid addiction and used to treat opioid use disorder oud.
FDA approval and medication classification
Sublocade received FDA approval on November 30, 2017, as an injectable formulation for treating opioid use disorder. This approval marked a significant milestone in treating opioid addiction, offering a new option for patients struggling with daily medication adherence. Sublocade is classified as a Schedule III controlled substance due to its moderate potential for abuse and is intended for patients who have already started treatment with a transmucosal buprenorphine product.
Buprenorphine, the active drug in Sublocade, functions as a partial opioid agonists. This means it activates brain’s opioid receptors in the brain but to a much lesser degree than full agonists like heroin or morphine. This partial activation is sufficient to reduce cravings and withdrawal symptoms without producing the intense euphoria associated with other opioids.
Recent FDA label changes for Sublocade now allow treatment to begin after a single dose of transmucosal buprenorphine.
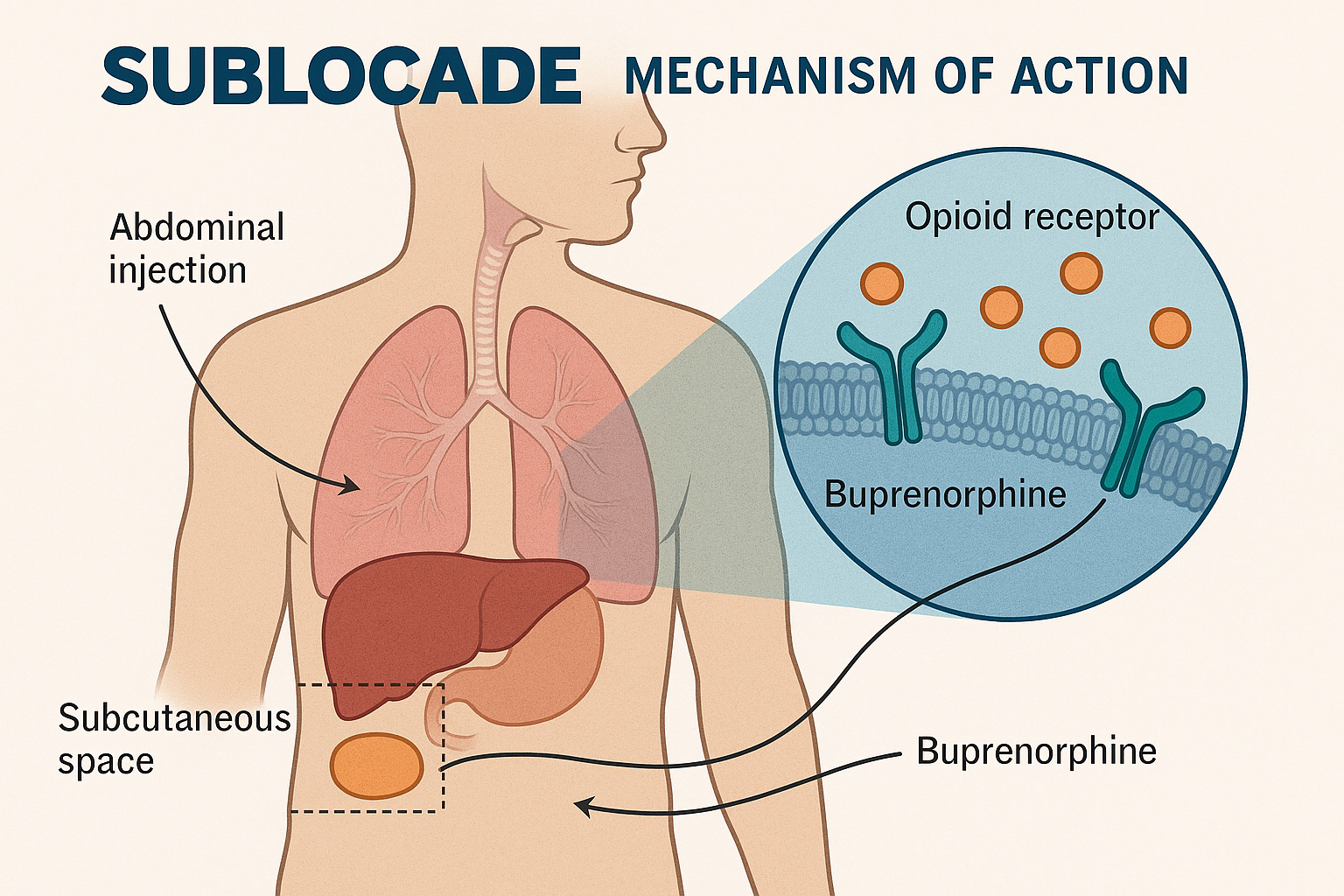
Mechanism of action
The mechanism of action for Sublocade involves the delivery of buprenorphine, which binds to opioid receptors in the brain. Sublocade works by:
- Alleviating withdrawal symptoms
- Reducing cravings by partially activating opioid receptors, thus aiding individuals in maintaining sobriety
- Blocking the effects of other opioids, preventing them from producing their euphoric and rewarding effects
Upon injection, Sublocade transforms into a solid gel, known as a depot, which gradually releases buprenorphine over 30 days. This ensures stable medication levels, minimizing fluctuations and maintaining therapeutic plasma levels throughout the month.
Clinical studies have demonstrated that Sublocade effectively prevents the rewarding effects of opioid drugs, making it a valuable tool in the fight against opioid addiction.
Sublocade vs Suboxone: What’s the difference?
When it comes to medication-assisted treatment for opioid addiction, Sublocade vs Suboxone are two prominent options with different administration methods and adherence benefits. While both medications contain buprenorphine, they differ significantly in their administration methods and dosing schedules. Sublocade is an injectable form of buprenorphine designed for once-monthly administration, whereas Suboxone is taken daily as a sublingual film or tablet.
These differences impact patient adherence, misuse risk, and treatment goals. Understanding the pros and cons of each HIV medications can help individuals and healthcare providers make informed decisions about which option is best suited for their needs.
In the following subsections, we will explore these differences in more detail.
Dosing and administration
Sublocade injection is administered as a subcutaneous injection once a month, typically in the abdomen, thigh, buttock, or upper arm. The initial dose is 300 mg, followed by a monthly maintenance dose that can be adjusted between 100 mg and 300 mg as needed. Monthly administration eliminates daily dosing, offering a convenient option for those struggling with daily medication adherence as part of the sublocade rems program.
In contrast, Suboxone is taken daily in film form under the tongue. Daily self-use requires consistent medication intake, which can be challenging for some. The monthly dosing of Sublocade simplifies the treatment regimen, reducing the burden on patients and improving overall adherence.
Risk of misuse or diversion
One of the significant advantages of Sublocade over Suboxone is the reduced risk of misuse and diversion. Because Sublocade is administered by a healthcare provider as a monthly injection, it cannot be taken orally or abused in the same way as oral buprenorphine. This helps ensure the medication is used as intended and reduces the likelihood of abuse.
However, it’s important to note that Sublocade is still a controlled substance and carries a risk of abuse similar to other opioids. Healthcare providers must monitor for signs of misuse and addiction, and educate patients on the dangers of self-administration and the importance of treatment adherence.
Patient suitability and treatment adherence
Sublocade is particularly beneficial for:
- Patients who have already stabilized on buprenorphine for at least a week, as this helps ensure a smoother transition to the injection.
- Individuals who have a history of relapse, as the steady release of medication can help mitigate cravings and withdrawal symptoms.
- Patients who prefer less frequent dosing, as Sublocade’s once-monthly injection is a more convenient alternative to daily medications.
On the other hand, Suboxone may be more suitable for individuals who are comfortable with daily medication routines and prefer the flexibility of self-administration. Ultimately, the choice between Sublocade and Suboxone depends on various factors, including lifestyle, severity of addiction, and adherence challenges.
Who should use Sublocade? Eligibility and patient criteria
Sublocade is specifically indicated for adults suffering from moderate to severe opioid dependence who have undergone prior treatment with oral buprenorphine for at least a week. This medication is intended for individuals who have shown they can tolerate buprenorphine and have demonstrated ongoing management of withdrawal symptoms. Transitioning to Sublocade offers patients the advantage of steady medication release and improved treatment adherence.
However, not everyone is a suitable candidate for Sublocade. Certain medical conditions and contraindications include:
- Severe respiratory problems
- Liver issues
- Known hypersensitivity to buprenorphine or any component of the delivery system These individuals should avoid using Sublocade.
Pre-treatment requirements
Before beginning treatment with Sublocade, patients must demonstrate ongoing management of withdrawal symptoms with a stable dose of oral buprenorphine for a minimum of seven days. This pre-treatment requirement ensures that patients can tolerate buprenorphine and helps prevent adverse reactions when transitioning to the injection format.
During the initial phase, patients receive a small dose of buprenorphine and are monitored for at least an hour to ensure they do not experience severe withdrawal symptoms. Careful monitoring helps healthcare providers determine the appropriate dosage and ensures a smooth transition to Sublocade.
Medical supervision and contraindications
Patients with certain medical conditions, such as severe respiratory problems or liver issues, should avoid using Sublocade as it may exacerbate their conditions. Individuals with a history of severe respiratory issues, liver problems, or those who are pregnant or breastfeeding should inform their healthcare provider before using Sublocade.
Additionally, Sublocade should not be administered to individuals who have a known hypersensitivity to buprenorphine or any component of the formulation. Healthcare providers must closely monitor patients for potential respiratory depression, especially if they are also taking benzodiazepines or other central nervous system depressants.
Sublocade dosage and administration process
Sublocade is administered as a subcutaneous injection, with options for the abdomen, thigh, buttock, or back of the upper arm. The initial dosage consists of two sublocade injections of 300 mg each, typically administered on the same day. Subsequent monthly maintenance doses should be given at least 26 days apart, with the dosage adjusted between 100 mg and 300 mg based on individual response.
If a patient misses a maintenance dose, it should be administered as soon as possible, with the next dose scheduled at least 26 days later. Once removed from refrigeration, Sublocade can remain at room temperature for up to 12 weeks before administration.
The buprenorphine injection used in Sublocade forms a depot under the skin, gradually releasing medication and maintaining therapeutic plasma levels throughout the month.
Benefits of using Sublocade for opioid addiction
One of the primary benefits of using Sublocade for opioid addiction is its ability to reduce the chance of missed doses and potential relapse compared to daily medications. The monthly administration ensures that patients receive a steady dose of medication, which can help reduce cravings and withdrawal symptoms, supporting long-term recovery.
Additionally, Sublocade’s injection format offers several benefits:
- Minimizes the risk of misuse and diversion, which are significant concerns with oral buprenorphine medications.
- Structured administration by healthcare professionals enhances treatment adherence.
- Provides a more controlled approach to opioid addiction treatment.
Sustained medication delivery
The formulation of Sublocade allows for the gradual release of buprenorphine over a month, ensuring consistent therapeutic levels in the bloodstream. This steady release helps block the pleasurable effects of opioids, reducing the likelihood of relapse and supporting long-term recovery.
The continuous delivery of medication by Sublocade minimizes plasma level fluctuations common with daily dosing options. This consistent delivery simplifies compliance for patients, minimizing the burden of daily dosing and improving overall treatment outcomes.
Clinical effectiveness and outcomes
Clinical studies indicate that the long-term use of buprenorphine, especially in injectable form like Sublocade, results in better treatment retention and fewer relapses.
- They have higher retention rates in treatment compared to those on daily oral medications.
- Patients receiving Sublocade are significantly more likely to achieve treatment success compared to those on placebo.
- 28% of patients on Sublocade achieve opioid-free status versus only 2% in the placebo group.
Combining Sublocade with counseling enhances treatment effectiveness, providing patients with long-term coping skills and emotional management strategies. A 12-week study was conducted on Sublocade. It effectively blocked the rewarding effects of opioids in individuals not seeking treatment.

Risks, side effects, and safety considerations
While Sublocade offers many benefits, it’s essential to be aware of the potential risks and side effects. The medication is administered through a restricted program due to the severe risk of harm from intravenous self-injection. Despite its controlled administration, patients may still experience side effects ranging from mild to severe.
Common side effects include nausea, constipation, fatigue, and injection site pain. More serious risks include liver enzyme elevations, respiratory depression, and dependency or withdrawal if discontinued improperly. A potential side effect to consider is the risk of respiratory depression.
Healthcare providers must closely monitor patients for any adverse reactions and provide appropriate medical supervision to manage these risks as healthcare professionals.
Common side effects
Patients receiving Sublocade may experience several common side effects. Nausea, constipation, fatigue, and injection site pain are frequently reported. Other side effects include headaches, itching at the injection site, and vomiting. Increased liver enzyme levels may also occur. Understanding how Sublocade affects patients is important for managing these symptoms.
While these side effects are typically mild, they can be bothersome for some patients, and a mild allergic reaction may occur. Individuals should communicate any discomfort to their healthcare provider to ensure appropriate management and support.
Serious risks and warnings
More serious risks associated with Sublocade include:
- Liver enzyme elevations
- Respiratory depression (rare)
- Severe allergic reactions, such as skin rashes, hives, or swelling, which require immediate medical attention.
The FDA has issued a boxed warning to alert doctors about the potential for severe respiratory depression and severe drowsiness, as well as other serious risks. Boxed warning alerts doctors about the need for close monitoring of patients, especially those on other central nervous system depressants, to prevent severe complications.
Sublocade cost, insurance coverage, and availability
The cost of Sublocade can be a concern for many patients:
- The monthly list price for Sublocade is $2,117.34.
- Most patients pay significantly less due to insurance and assistance programs.
- Patients with commercial insurance typically have out-of-pocket costs ranging from $0.01 to $1,993 per month.
Medicaid patients may pay as little as $1 to $4 per month, depending on their state plan, while Medicare beneficiaries might incur costs between $0.02 and $1,607 per dose. The INSUPPORT Copay Assistance Program helps eligible patients reduce their monthly costs for Sublocade to as little as $0.
It’s important to note that Sublocade is not available at retail pharmacies and must be administered by a certified healthcare provider.
How to get started with Sublocade
Starting treatment with Sublocade involves several steps:
- Begin with an evaluation by a healthcare provider.
- Patients must first be stabilized on a dose of oral buprenorphine.
- Transition to Sublocade after stabilization.
This initial phase ensures that patients can tolerate buprenorphine and are suitable candidates for the injection.
Once stabilized, patients will receive a 300 mg dose of Sublocade during their initial appointment. Subsequent doses are administered as monthly injections, with healthcare providers scheduling regular appointments to monitor progress and adjust the dosage as needed.
Finding a certified Sublocade provider
Finding a certified provider to administer Sublocade is a crucial step in starting treatment. Only certified healthcare providers can prescribe and administer Sublocade, as it is not available in retail pharmacies. Patients can locate a qualified provider using the ‘Find a Treatment Provider’ tool or by calling INSUPPORT.
The search for a Sublocade treatment provider can be customized based on the user’s current location or ZIP code. This tool lists healthcare professionals authorized to prescribe Sublocade, ensuring they have met the necessary requirements to administer the medication safely.
Bottom line: What is Sublocade
Sublocade represents a significant advancement in the treatment of opioid addiction, offering a convenient and effective option for individuals seeking long-term recovery. By providing a steady release of buprenorphine over 30 days, Sublocade helps reduce cravings and withdrawal symptoms, supporting sustained sobriety.
While Sublocade offers many benefits, it is essential to consider the potential risks and side effects. Close medical supervision and adherence to prescribed treatment protocols are crucial for achieving the best outcomes. If you or a loved one is struggling with opioid addiction, Sublocade may be a valuable tool in the journey to recovery. Consult with a healthcare provider to determine if Sublocade is the right choice for you.
FAQs about Sublocade
Can I stop Sublocade anytime?
You should not stop Sublocade treatment abruptly, as it can cause withdrawal symptoms and increase the risk of relapse. Always consult with your healthcare provider for guidance on managing your treatment.
How long should I stay on Sublocade?
The length of time you should stay on Sublocade is determined by your healthcare provider based on your individual progress and response to the medication. It's important to follow their guidance for the best results.
What happens if I miss a dose?
If you miss a dose of Sublocade, take it as soon as you remember, but ensure the next dose is scheduled at least 26 days later to maintain consistent medication levels.
Can Sublocade be obtained at retail pharmacies?
Sublocade cannot be obtained at retail pharmacies; it must be administered by a certified healthcare provider.
Are there any restrictions on using other medications while on Sublocade?
Yes, there are restrictions on using other medications while on Sublocade due to potential serious interactions. It's crucial to inform your healthcare provider of all medications, including over-the-counter drugs and supplements, to ensure safety.
















