Many drugs can impact digestive health, causing issues like constipation, diarrhea, and nausea. This article explores how drugs impact digestive health through different medications, including opioids, NSAIDs, and antibiotics, and which symptoms to watch out for.
Key Takeaways
- Many drugs, including opioids, NSAIDs, and antibiotics, can negatively impact digestive health, causing issues like constipation, ulcers, and microbiome disruption.
- Short-term and long-term medication use may lead to varying digestive side effects; understanding these can aid in effective management of gastrointestinal issues.
- Preventive strategies, such as dietary adjustments, hydration, and the use of probiotics, are essential for maintaining digestive health while on medication.
Do drugs negatively affect digestive health?
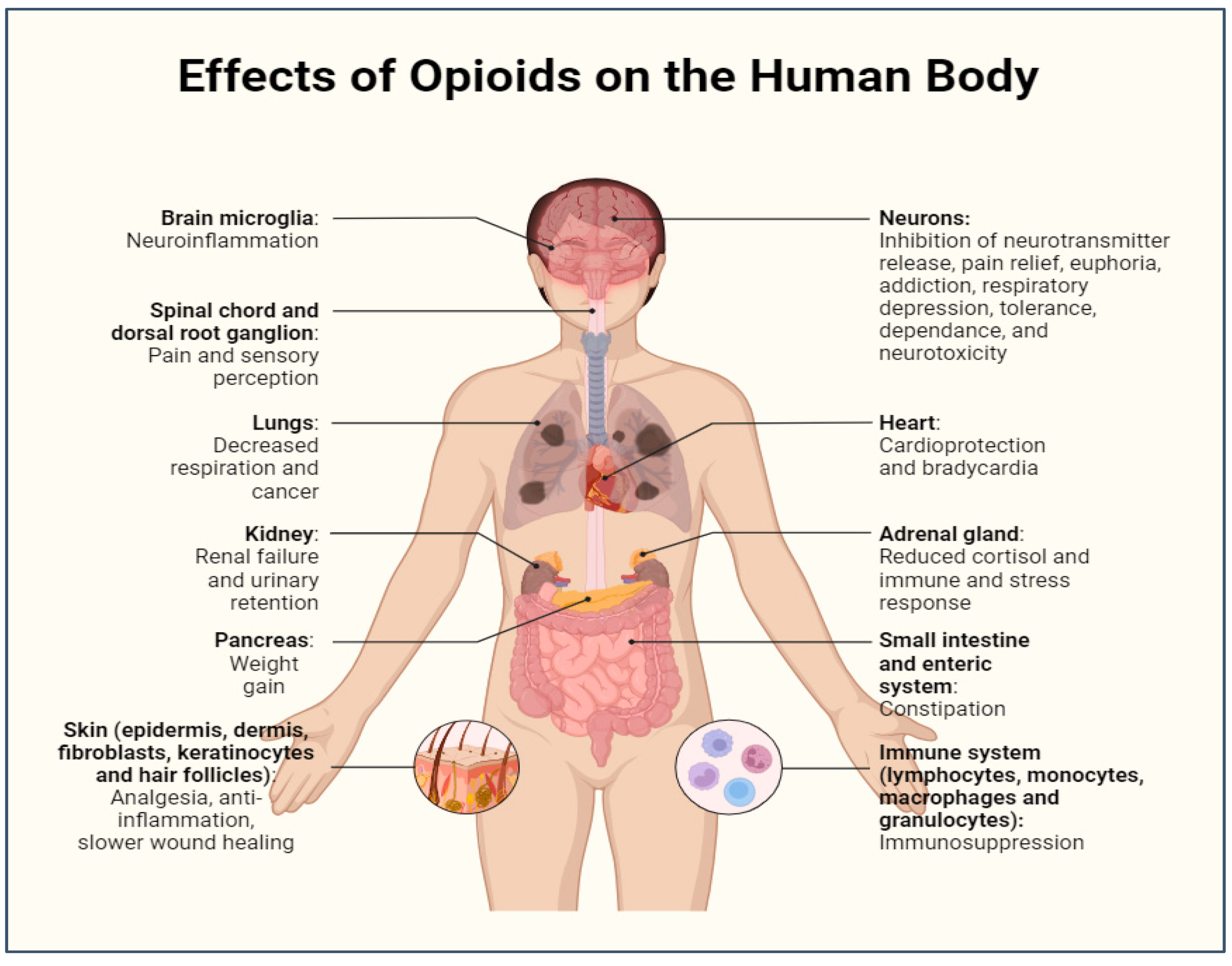
The answer is a resounding yes. Many drugs can negatively impact digestive health, leading to a range of gastrointestinal issues. Opioids, for instance, are notorious for causing opioid-induced bowel dysfunction, which includes symptoms like constipation and abdominal pain. NSAIDs can damage the gut lining, leading to ulcers and bleeding.
Antibiotics, while crucial for fighting infections, can disrupt the gut microbiome, causing diarrhea and other digestive disturbances. Even antacids and psychiatric medications are not without their adverse effects on the digestive system. These medications can slow motility, alter microbial balance, and damage mucosal linings, creating a cascade of digestive issues that can significantly affect quality of life.
Main drug categories linked to digestive side effects
Several drug categories are notably linked to digestive side effects. Opioids, including Suboxone and other opioids, are well-known for causing opioid-induced bowel dysfunction, which slows down gastrointestinal motility and often results in constipation.
Medications and their effects on the gut include:
- Antibiotics: can disrupt the gut microbiome, leading to diarrhea and other digestive issues.
- NSAIDs (such as ibuprofen and naproxen): can damage the gut lining, increasing the risk of ulcers and GI bleeding.
- Antacids, particularly PPIs: can alter stomach acid levels, promoting bacterial overgrowth.
Psychiatric medications, including SSRIs, can affect the gut-brain axis, impacting both gut motility and mental health. Knowing these categories and their effects helps in managing gastrointestinal issues effectively.
Common symptoms caused by drug-related digestive issues
Drug-related digestive issues manifest in various symptoms, commonly including:
- Constipation
- Bloating
- Nausea
- Acid reflux
- Diarrhea
For instance, taking Suboxone can lead to severe constipation, characterized by straining, lumpy stools, and infrequent bowel movements—an issue covered in our guide on does Suboxone cause constipation. Some individuals may experience diarrhea, which can be disruptive to daily activities, and it is important to be aware of the side effects of Suboxone that affect digestive function.
Common symptoms affecting digestive health include:
- Nausea, which can significantly affect one’s quality of life.
- Acid reflux, often exacerbated by certain medications, leading to persistent discomfort and digestive health challenges.
- Bloating, causing discomfort and affecting overall well-being, which may be associated with various health conditions.
Identifying these symptoms is the first step in effective management.
Which drugs are worst for gut health?
Certain medications are particularly harmful to gut health, and understanding their impacts can help in managing gastrointestinal issues effectively. The worst offenders include:
- Opioids
- NSAIDs
- Antibiotics
- PPIs These drugs can severely impact gut function, leading to a range of digestive health issues.
Opioids, for instance, disrupt motility and cause constipation, while NSAIDs can damage the gut lining and lead to ulcers. Antibiotics often result in a microbiome imbalance, causing diarrhea, and PPIs can promote bacterial overgrowth when overused. Knowing these drugs and their adverse effects helps maintain digestive health.

Opioids: Disrupting motility and causing constipation
Opioids are notorious for disrupting gut motility and causing constipation, a condition commonly referred to as opioid-induced bowel dysfunction. These drugs bind to opioid receptors in the gastrointestinal tract, slowing peristalsis and reducing fluid secretion, which leads to bowel movement issues.
Suboxone use, for example, often causes gastrointestinal issues like nausea and constipation due to its opioid content, specifically buprenorphine. For more details, see our full guide on gut health and Suboxone. To alleviate constipation, the following are recommended: suboxone treatment - Increasing dietary fiber intake - Increasing fluid intake - Using over-the-counter stool softeners - Using osmotic laxatives
Knowing these mechanisms aids in managing opioid use side effects.
NSAIDs: Gut lining damage and ulcers
NSAIDs, such as ibuprofen and naproxen, can cause significant damage to the gut lining, leading to ulcers and gastrointestinal bleeding. These drugs:
- Inhibit prostaglandins, which are crucial for maintaining the protective mucosal stomach lining of the gut
- Cause mucosal injury
- Increase the risk to develop stomach ulcers
Long-term NSAID users may develop endoscopic abnormalities, including mucosal erosions, even if they do not exhibit dyspeptic symptoms. Selective COX-2 inhibitors are less likely to cause gastrointestinal damage compared to traditional non-selective NSAIDs.
Knowing these risks helps manage gastrointestinal issues from NSAID use.
Antibiotics: Microbiome imbalance and diarrhea
Antibiotics, especially broad-spectrum ones like amoxicillin and ciprofloxacin, can disrupt the natural balance of gut bacteria, leading to diarrhea and other digestive issues. This disruption, known as dysbiosis, often results in antibiotic-associated diarrhea (AAD). The imbalance created in the gut microbiota can also increase susceptibility to infections like Clostridium difficile. Long-term antibiotic use may lead to the development of antibiotic-resistant bacteria, posing additional health risks.
Restoring gut health after antibiotic use can be supported through the use of probiotics, which help repopulate beneficial bacteria.
Proton Pump Inhibitors (PPIs): Overuse and bacterial overgrowth
Proton Pump Inhibitors (PPIs), such as omeprazole, are commonly used to treat acid reflux but can lead to bacterial overgrowth when overused. Long-term PPI use alters stomach acid levels, promoting small intestinal bacterial overgrowth (SIBO) and impairing nutrient absorption.
While PPIs decrease gastric acid, which theoretically increases the risk of infections like C. difficile, actual rates of bacterial overgrowth were not significantly different among users and non-users. Patients at high risk for bacterial overgrowth or C. difficile infection should be carefully evaluated before being prescribed PPIs.
Understanding these risks can help manage the adverse effects of PPI use effectively.
How drugs alter the gut microbiome
The gut microbiome, a complex community of trillions of microorganisms, plays a crucial role in how drugs are metabolized and how intestines absorb them. Disruption of this microbial balance is a central mechanism for many drug-related digestive issues in the digestive tract. Antibiotics, for instance, can drastically shift gut bacteria, reducing microbial diversity and leading to digestive problems.
Psychiatric medications, like SSRIs and antipsychotics, can also affect the gut-brain axis, influencing both mood and digestion. This becomes even more important when evaluating Suboxone interactions with other drugs. Understanding these interactions can help in managing gastrointestinal issues effectively.

Microbiome shifts caused by antibiotics
Antibiotics can lead to significant changes in gut bacteria, often resulting in digestive problems and reduced microbial diversity. Broad-spectrum antibiotics are particularly linked to a higher risk of developing infections like Clostridioides difficile due to the depletion of beneficial gut bacteria, such as Bifidobacterium and Lactobacillus.
Exposure to antibiotics during early life can affect the development of the gut microbiota, potentially leading to long-term health issues such as obesity and asthma. These changes can impact metabolic functions, including the synthesis of essential metabolites. Knowing these shifts aids in managing antibiotic use side effects.
Impact of psychiatric medications on gut-brain axis
Psychiatric medications, including SSRIs and antipsychotics, can alter the gut-brain axis, affecting gut health and potentially influencing mood and overall digestion. These medications can induce notable shifts in gut microbiota diversity, which can vary depending on the specific medication used, impacting mental health and emotional regulation.
The gut-brain axis is a bidirectional communication system that allows psychotropic drugs to influence gastrointestinal functions and microbiota composition. Research indicates that probiotics and prebiotics may enhance the efficacy of psychiatric treatments by positively modulating gut microbiota. Knowing these effects helps manage gastrointestinal issues from psychiatric medication use.
Short-term vs. long-term digestive side effects of medications
Medications can cause both short-term and long-term digestive side effects, and understanding these differences is crucial. Short-term use of some medications can provide quick relief from digestive issues but may lead to side effects like nausea and stomach cramps. For instance, a one-time use of NSAIDs might result in temporary stomach discomfort.
However, long-term reliance on medications like opioids can alter gut flora, leading to chronic issues such as constipation and opioid-induced bowel dysfunction, as noted in our guide on long-term Suboxone use. Long-term use of PPIs is linked to deficiencies in essential nutrients such as magnesium and vitamin B12. Knowing these effects aids in effective gastrointestinal issue management.
What to do if medications are causing digestive problems
If you experience digestive problems while on medication, it is crucial to:
- Recognize and report these issues to your healthcare provider.
- Understand that early identification helps manage gastrointestinal issues before they escalate.
- Keep a detailed record of symptoms and any relevant medication details to facilitate effective communication with your doctor.
This proactive approach ensures prompt addressing of any adverse effects on the digestive system.
How to discuss concerns with your doctor
Open communication with your healthcare provider is vital for dealing with drug-related digestive issues and prescription medications. Prepare a list of your symptoms and any medication details before your appointment.
Openly discussing your concerns helps your doctor understand the issue better for a better understanding and recommend alternatives, dosage changes, or additional treatments. This dialogue is crucial for managing gastrointestinal issues effectively.
Possible medication substitutes with fewer digestive side effects
There are alternative medications and other medications available that have a lower likelihood of causing gastrointestinal discomfort. For instance, acetaminophen can be used instead of NSAIDs to reduce the risk of stomach issues.
Herbal remedies like peppermint oil and Iberogast have shown effectiveness in alleviating IBS symptoms. Mind-body therapies such as yoga and cognitive behavioral therapy offer benefits in managing symptoms without typical medication side effects.
Probiotics are increasingly recognized for their benefits in digestive health, providing a non-pharmaceutical option for managing symptoms. Exploring these alternatives can help manage gastrointestinal issues effectively.
Preventing digestive issues while on medication
Preventing digestive issues while on medication involves evidence-based strategies tailored to different drug types. Regular physical activity can aid in digestion and reduce medication-related gastrointestinal issues. Implementing dietary adjustments, such as incorporating high-fiber foods and staying hydrated, can support digestive health.
Knowing these preventive measures aids in managing GI problems and gastrointestinal issues.
Dietary adjustments and hydration strategies
Dietary adjustments and hydration strategies are crucial for maintaining digestive health while on medication. A high-fiber diet, rich in fruits and vegetables, can enhance fiber intake and support digestive function. Drinking plenty of fluids throughout the day helps prevent constipation and maintains overall digestive health.
Regular meal timing can also prevent digestive disturbances and promote gut health. These dietary and hydration strategies can significantly reduce medication-related gastrointestinal issues.
Use of probiotics and gut support supplements
Probiotics and gut support supplements can play a significant role in maintaining gut health during medication use. Specific strains like Lactobacillus rhamnosus GG and Saccharomyces boulardii are known to help maintain microbial balance and alleviate antibiotic-associated diarrhea. Prebiotic fibers can enhance the effectiveness of probiotics and promote overall gut health.
Using these supplements can improve digestion and decrease the occurrence of medication-induced gastrointestinal side effects. Knowing the benefits of probiotics and gut support supplements aids in effective gastrointestinal issue management.
When to seek medical attention for drug-related digestive symptoms
Recognizing when to seek medical attention for drug-related digestive symptoms is crucial for preventing serious complications. Red flag symptoms include:
- Severe stomach pain
- Persistent vomiting
- Lightheadedness
- Dizziness
- Blood in vomit or stools
- Symptoms that persist for more than a week
These symptoms could indicate serious conditions like ulcers or gastrointestinal bleeding.
If you experience any of these symptoms, it is essential to contact your healthcare provider immediately to address the issue and prevent further complications.
Bottom Line: Monitoring digestive health on medication
Monitoring digestive health while on medication is crucial for identifying and managing any adverse effects early on. Advancements in wearable technology and mobile health apps enable continuous monitoring of gastrointestinal function, which contributes to better health outcomes. Patients are encouraged to actively participate in tracking their symptoms and maintaining open communication with their healthcare providers.
Proactive management, including personalized dietary strategies and the use of probiotics, can significantly improve digestive health during long-term medication use. Knowing these approaches helps manage gastrointestinal issues effectively.
FAQs on drugs and digestive health
Can antidepressants cause IBS symptoms?
Indeed, certain antidepressants, especially SSRIs, can influence gut motility and exacerbate IBS symptoms by affecting the gut-brain axis. Therefore, it is crucial to monitor any gastrointestinal changes when on these medications.
Is it safe to take PPIs long term?
Long-term use of PPIs is not considered entirely safe due to potential risks such as bacterial overgrowth and deficiencies in essential nutrients like magnesium and vitamin B12. It is crucial to utilize them under medical supervision.
How can I alleviate constipation caused by opioids?
Increasing your dietary fiber and fluid intake is essential for alleviating opioid-induced constipation. Additionally, over-the-counter stool softeners or osmotic laxatives may provide effective relief.
What are the alternatives to NSAIDs for pain relief?
Acetaminophen and herbal remedies such as peppermint oil serve as effective alternatives to NSAIDs for pain relief, offering benefits like reduced gastrointestinal side effects.
Can probiotics help with antibiotic-associated diarrhea?
Probiotics, such as Lactobacillus rhamnosus GG and Saccharomyces boulardii, are effective in restoring microbial balance and reducing antibiotic-associated diarrhea. Therefore, incorporating these probiotics may be beneficial during antibiotic treatment.
















