If you’re taking Suboxone, knowing its interactions with drugs, alcohol, food, and supplements is essential, especially regarding suboxone interactions. This article explains how these interactions can impact your treatment and what you need to avoid to stay safe.
Key Takeaways
- Suboxone consists of buprenorphine and naloxone, which work together to treat opioid dependence by reducing withdrawal symptoms and preventing misuse.
- Awareness of potential drug, food, and alcohol interactions with Suboxone is crucial to avoid severe side effects and ensure safe treatment, particularly with CNS depressants.
- Patients should maintain open communication with healthcare providers regarding their medications and any supplements to manage interactions and optimize treatment effectiveness.
What is Suboxone, and how does it work?
Suboxone is a medication specifically designed to treat opioid addiction, helping reduce withdrawal symptoms and prevent relapse. Comprising buprenorphine and naloxone, Suboxone offers a dual approach to managing opioid addiction. Buprenorphine treatment is a partial opioid agonist, which means it binds to opioid receptors in the brain to alleviate withdrawal symptoms and cravings without causing significant intoxication.
The second component, a drug called naloxone, is an opioid antagonist included to deter misuse. If someone attempts to inject or snort Suboxone, naloxone triggers withdrawal symptoms, thus discouraging abuse. When taken as prescribed, buprenorphine naloxone minimizes withdrawal effects and blocks other opioids from binding to the same receptors, making it an effective barrier against relapse.
Patients must usually discontinue other opioids before beginning Suboxone treatment to allow opioid withdrawal symptoms to appear, making the medication effective. Knowing how Suboxone interacts with other substances is crucial for safe and successful treatment.

Why understanding Suboxone interactions is essential
Awareness of Suboxone drug interactions is essential to prevent severe adverse reactions. Combining Suboxone with specific medications can cause life-threatening side effects, so knowing which substances to avoid is crucial.
Patients should identify substances that can interfere with Suboxone treatment to maintain its efficacy and safety. For instance, sedating medications can cause increased respiratory depression when taken with Suboxone, highlighting the need for careful management.
Knowledge of potential drug interactions allows healthcare providers to create safer treatment plans, ensuring effective management of opioid drugs dependency with minimized adverse effects. Patient education on certain drug interactions promotes treatment adherence and improves recovery outcomes.
Drug interactions with Suboxone
Suboxone interacts with several classes of medications, primarily through mechanisms like central nervous system (CNS) depression and enzyme inhibition. Benzodiazepines, such as Xanax and Valium, are particularly risky as they enhance CNS depression, leading to potentially fatal respiratory issues.
Medications that can interact with Suboxone and require careful monitoring include:
- Antidepressants, such as SSRIs, SNRIs, and tricyclics
- Antipsychotics
- Antibiotics
- Antifungals
- Seizure medications
These medications can affect the metabolism of Suboxone, altering its efficacy and safety.
The FDA warns about high-risk interactions between Suboxone and other opioids or partial agonists, which can cause overdose or reduced treatment effectiveness. Knowing buprenorphine drug interactions is crucial for Suboxone patients. If you’re unsure, here’s a guide on what medications can you not take with Suboxone that should be avoided or monitored closely.
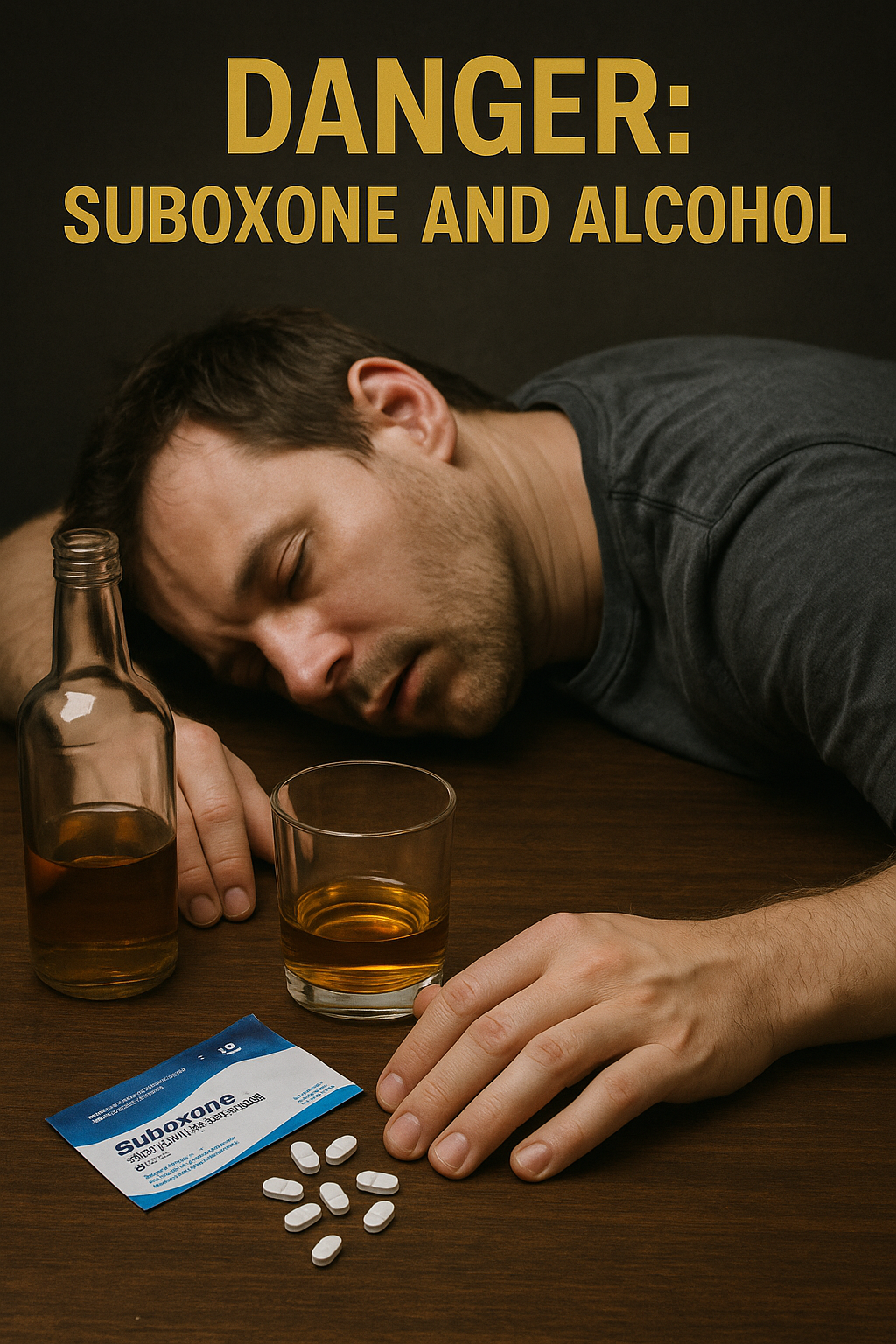
Suboxone and alcohol: A dangerous combination
Alcohol is another central nervous system depressant, and when combined with Suboxone, it can significantly enhance each other’s effects, especially in individuals with alcohol dependence. This combination can lead to severe side effects like nausea, dizziness, and impaired judgment.
More alarmingly, mixing Suboxone with alcohol can cause respiratory depression, coma, and even death, especially for individuals with a history of alcohol addiction. Long-term use of both substances together may result in respiratory issues and potentially serious brain damage due to decreased oxygen flow.
Due to these risks, completely avoiding alcohol while on Suboxone is essential. Even moderate alcohol can cause extreme fatigue and a higher risk of unconsciousness, with dangers far outweighing any potential enjoyment.
Suboxone food interactions: What to avoid or consider
Food does not significantly affect the absorption of Suboxone, which means you can generally eat without worrying about altering the medication’s effectiveness. However, grapefruit and grapefruit juice can act as enzyme inhibitors (CYP3A4) and may alter Suboxone levels in your system.
Additionally, while caffeine and other substances have minor interactions, they are usually not significant enough to cause concern. It’s wise to discuss your diet and any concerns with your healthcare provider to avoid other interactions.
Suboxone and over-the-counter (OTC) medications
Certain over-the-counter (OTC) medications can increase drowsiness or mask symptoms of an overdose when taken with Suboxone. Common OTC meds to watch out for include sedating antihistamines like diphenhydramine and cold medications with dextromethorphan and acetaminophen combinations.
These interactions are particularly dangerous because they can exacerbate the sedative effects of Suboxone, leading to severe respiratory depression, breathing problems, or other serious side effects. Consult your healthcare provider before taking any OTC medications while on Suboxone.
Suboxone and supplements or herbal products
Supplements and herbal products can also interact with Suboxone, leading to increased sedation or interference with the medication’s metabolism. Common supplements that may interact include St. John’s Wort, an enzyme inducer, and CNS depressants like valerian root and melatonin.
Consult a healthcare provider before using any supplements or herbal products while on Suboxone to avoid harmful interactions. This step ensures that your treatment remains effective and safe.
Patient-specific risks with Suboxone interactions
Certain medical conditions can exacerbate the risks associated with Suboxone interactions. For example, individuals with respiratory problems may face increased risks of severe side effects. Those with liver conditions require careful monitoring, as Suboxone can worsen liver problems or alter its metabolism.
Patients with a history of head injuries should be cautious, as Suboxone can increase pressure in the brain. Additionally, individuals with mental health issues may experience worsened symptoms when taking Suboxone.
Individualized medical supervision and ongoing monitoring are vital given these patient-specific risks. Pregnant individuals and those with a history of alcohol use disorder should also discuss their treatment options thoroughly with their healthcare providers, especially if they are dealing with substance use disorder and substance abuse.
What to do if you suspect a harmful interaction
If you suspect a harmful interaction while taking Suboxone, it is essential to know the warning signs and when to seek emergency medical help. Signs such as slowed breathing, extreme drowsiness, and confusion may signal a Suboxone overdose and require immediate medical attention.
For non-emergency interactions, consult your prescribing clinician promptly to discuss symptoms and adjust your suitable treatment plan if necessary. Open communication with your healthcare provider is key to managing your treatment safely, especially when a doctor prescribes to treat anxiety.
How to manage Suboxone safely alongside other medications
Managing suboxone medication safely with other medications involves key steps: maintain a comprehensive list of all medications and supplements, and share it with every healthcare provider to prescribe suboxone and avoid potential interactions.
Avoid self-medicating or adding new drugs without consulting your healthcare provider. Regularly review all your frequently prescribed medications and your medication guide for prescription drug and other frequently prescribed medications and supplements with your provider to ensure ongoing safety and treatment efficacy.
Pharmacist consultations and medication reconciliations at each visit can further minimize the risks of harmful interactions. This proactive approach ensures that your Suboxone treatment remains effective and safe.

Bottom Line: Suboxone interactions and your recovery journey
Successfully managing Suboxone interactions is key to a safe and effective recovery journey. Understanding the potential risks and taking proactive steps when starting suboxone treatment can optimize your treatment and enhance your chances of long-term recovery.
Communicate openly with your medical provider and adhere to their recommendations. Your commitment to managing interactions significantly impacts your clinical importance, treatment success, and overall well-being.
FAQs About Suboxone Interactions
What are the main components of Suboxone?
Suboxone consists mainly of buprenorphine, a partial opioid agonist, and naloxone, an opioid antagonist, working together to treat opioid dependence effectively.
Why should I avoid alcohol while taking Suboxone?
You should avoid alcohol while taking Suboxone because both substances are central nervous system depressants, and their combination can result in severe respiratory depression, coma, or even death. Prioritizing your safety is essential.
Can I take over-the-counter medications with Suboxone?
It is crucial to consult your healthcare provider before taking over-the-counter medications with Suboxone, as some may increase drowsiness or mask overdose symptoms. Prioritizing safety is essential when managing your health.
What foods should I avoid while taking Suboxone?
You should avoid grapefruit and grapefruit juice while taking Suboxone, as they can alter medication levels. It is advisable to consult with your healthcare provider regarding your diet for optimal treatment outcomes.
What should I do if I suspect a harmful interaction with Suboxone?
If you suspect a harmful interaction with Suboxone, seek emergency medical help for severe symptoms such as slowed breathing or extreme drowsiness. For less urgent situations, promptly consult your prescribing clinician.
















