Buprenorphine helps manage opioid addiction by partially activating opioid receptors in the brain. This reduces cravings and withdrawal symptoms without causing intense euphoria. This article explains how buprenorphine works in the body and what makes it effective and safe.
Key Takeaways
- Buprenorphine is a partial opioid agonist, activating mu-opioid receptors to relieve pain and manage cravings while minimizing the risk of overdose due to its ceiling effect.
- The drug’s extended half-life allows for less frequent dosing, providing stable maintenance therapy for opioid dependence, while its sublingual formulation enhances bioavailability.
- Buprenorphine’s unique properties, including its ability to block the effects of other opioids and stabilize mood, support effective addiction treatment and differentiate it from full opioid agonists.
What does buprenorphine do in the body?
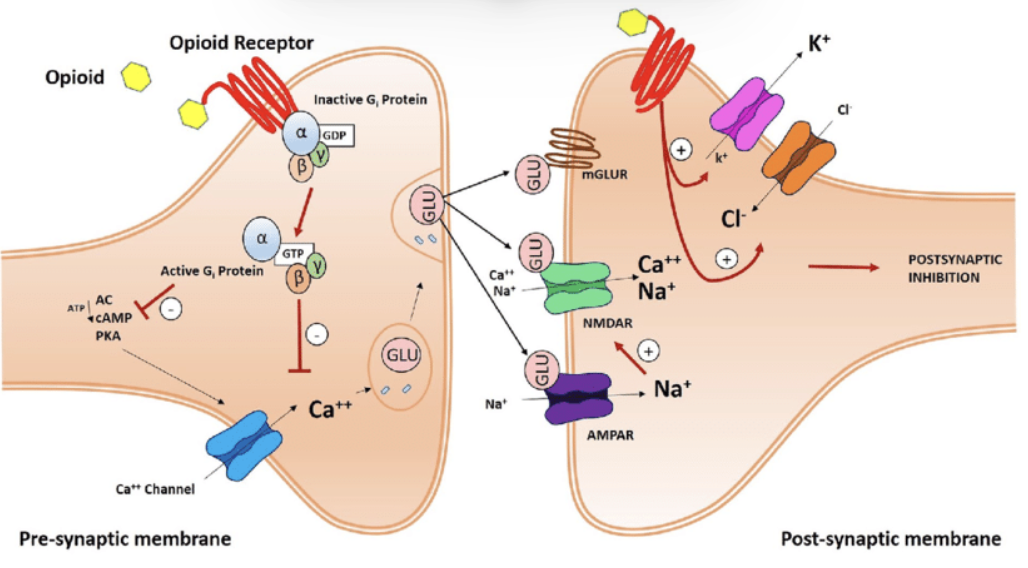
Buprenorphine is integral to opioid addiction treatment, functioning as a partial opioid agonist. It activates mu-opioid receptors in the brain, albeit less intensely than full opioid agonists like heroin or oxycodone, which helps relieve pain and curb cravings without causing significant euphoria. This partial activation helps manage opioid withdrawal symptoms effectively, making it easier for individuals to transition away from more harmful opioid use.
Furthermore, buprenorphine’s unique pharmacological profile includes a ceiling effect, which limits its effects at higher doses. This characteristic significantly reduces the risk of overdose, a common and often fatal issue with full opioid agonists.
Understanding buprenorphine’s interaction with opioid receptors and its advantages over other treatments enables patients and healthcare providers to make informed decisions about managing opioid addiction.

Buprenorphine binds to mu-opioid receptors
Buprenorphine’s interaction with the mu opioid receptor is central to its effectiveness in treating opioid dependence. As a partial agonist, it binds to these receptors and partially activates them, resulting in reduced cravings and withdrawal symptoms without causing a strong euphoric effect. This partial activation helps stabilize mood and alleviate the emotional fluctuations often experienced during opioid withdrawal.
Moreover, buprenorphine has a high affinity for mu-opioid receptors, meaning it binds more strongly than many full agonists. This strong binding not only helps block the effects of other opioids but also contributes to its prolonged duration of action, making it effective for long-term maintenance therapy.
Understanding these mechanisms allows patients to appreciate how buprenorphine helps manage cravings and maintain stability during recovery.
Ceiling effect reduces overdose risk
One of buprenorphine’s most significant safety features is its ceiling effect:
- After reaching a certain dose, increasing the dosage does not proportionally increase its effects.
- This ceiling effect is particularly beneficial in reducing the risk of respiratory depression, a common cause of death in opioid overdoses.
- Unlike full opioid agonists, which continue to increase in effect as the dose rises, buprenorphine levels off.
- This provides a built-in safeguard against overdose.
This property makes buprenorphine a safer option for long-term use of buprenorphine in managing opioid dependence. When used alone and not combined with other sedatives, the risk of overdose is extremely minimal.
Suboxone, a combination of buprenorphine and naloxone, leverages this ceiling effect while also incorporating naloxone to deter misuse and reduce overdose potential. Understanding this feature can help patients and healthcare providers feel more confident in the safety of buprenorphine therapy.
How long does buprenorphine stay in your system?
Buprenorphine’s duration in the system can vary, but it generally produces effects for about 24 to 60 hours. However, it may remain detectable in drug tests for up to 7 to 10 days, depending on individual metabolism and dosage. This extended presence in the body is due to its long half-life, which supports stable dosing schedules and effective treatment.
Knowing buprenorphine’s pharmacokinetics helps manage treatment schedules and anticipate urine drug screening results, aiding patients and healthcare providers in planning dosage adjustments and monitoring compliance.
Half-life and duration of action
Buprenorphine has a variable half-life ranging from 24 to 42 hours, with an average of about 38 hours. This extended half-life allows for less frequent dosing, which can be beneficial for individuals in long-term treatment for opioid dependence. The effects of buprenorphine can last much longer than its half-life suggests due to its pharmacological properties, providing sustained relief from withdrawal symptoms.
Patients can often achieve stable drug levels with consistent daily dosing, and in some cases, a buprenorphine dose can be prescribed on alternate days once a patient’s clinical stability permits. This flexibility can enhance adherence to treatment plans and improve overall outcomes for individuals managing opioid dependence.
Metabolism and excretion
Buprenorphine pharmacokinetic is primarily metabolized in the liver through the cytochrome P450 enzyme system, specifically by CYP3A4 enzymes. This hepatic metabolism converts buprenorphine into norbuprenorphine, an inactive metabolite, which is then excreted through urine and feces. The drug’s significant first-pass effect reduces its bioavailability when taken orally, making buprenorphine administered sublingual administration more effective.
The elimination of buprenorphine primarily occurs through feces, with less than 20% being excreted via the kidneys. This highlights the importance of liver function in buprenorphine clearance. Knowing these metabolic and excretion pathways aids in tailoring treatment to individual patient needs, especially those with liver impairments.
Buprenorphine’s mechanism of action explained
Buprenorphine’s mechanism of action is distinct from full opioid agonists and antagonists. As a partial agonist at mu-opioid receptors, it provides moderate activation that leads to dopamine release without significant respiratory depression. This partial activation helps manage pain and reduce cravings, making buprenorphine an effective treatment for opioid dependence.
In addition to its partial agonist activity, buprenorphine also exhibits antagonist properties at other opioid receptors, contributing to its unique therapeutic profile and partial agonist properties. Knowing these mechanisms helps patients and healthcare providers better appreciate buprenorphine’s role in opioid addiction treatment.
Partial agonist activity
As a partial agonist, buprenorphine:
- Activates opioid receptors but to a lesser extent than full agonists like heroin or methadone.
- Produces a ceiling effect through controlled activation, limiting the extent of its effects and lowering the risk of overdose.
- Displaces full agonists from the mu receptors, allowing it to reduce the effects of stronger opioids and manage withdrawal symptoms effectively.
The partial agonist nature of buprenorphine also contributes to its reduced potential for abuse and lower physical dependence compared to full agonists. This makes it a safer and more manageable option for long-term treatment of opioid dependence.
Antagonist properties at other receptors
Buprenorphine also acts as an opioid antagonist at kappa-opioid receptors, which can help stabilize mood and reduce dysphoria. Blocking these receptors helps buprenorphine mitigate feelings of anxiety and discomfort, contributing to emotional stability during recovery.
This antagonistic effect on kappa receptors is an added benefit, as it helps alleviate negative mood states and supports overall mental health in individuals undergoing opioid addiction treatment. Understanding these dual actions of buprenorphine can provide a more comprehensive view of its therapeutic potential.
Buprenorphine vs. other opioids: What makes it different?
Buprenorphine stands out from other opioids due to its partial agonist nature, which provides a unique advantage in managing opioid dependence:
- Unlike full agonists like heroin or methadone, buprenorphine produces effects that are less intense.
- This reduces the potential for abuse and overdose.
- These properties make it a preferred option for long-term maintenance therapy.
Comparing buprenorphine to other opioids highlights its safety profile and effectiveness in treating opioid addiction. Knowing these differences helps patients and healthcare providers select the most suitable treatment for managing opioid dependence.
Buprenorphine vs. methadone
Compared to methadone, which is a full opioid agonist, buprenorphine offers a safer profile with a lower overdose risk, a key distinction in the suboxone vs methadone treatment debate. Methadone is a full agonist that provides stronger effects but also has a higher potential for overdose. Buprenorphine’s ceiling effect reduces the risk of respiratory depression and overdose, making it a safer option for many patients.
Additionally, buprenorphine can be prescribed in various settings, including outpatient environments, whereas methadone typically requires administration in structured clinics. This flexibility can make buprenorphine more accessible and convenient for patients, enhancing adherence to treatment plans and allowing providers to dispense buprenorphine more effectively.
Buprenorphine vs. heroin or oxycodone
Buprenorphine’s effects are milder compared to full agonists like heroin or oxycodone, which helps in alleviating withdrawal symptoms without inducing intense highs. By effectively attaching to mu-opioid receptors, buprenorphine blocks the effects of stronger opioids and can precipitate opioid withdrawal signs while supporting recovery.
This partial activation helps reduce cravings and manage withdrawal symptoms, making it a crucial component of opioid addiction treatment. Understanding these differences underscores buprenorphine’s role in effective opioid addiction treatment, offering a safer and more controlled approach to recovery.
What are the effects of buprenorphine on the brain and nervous system?
Buprenorphine impacts brain function by altering pain perception and affecting neurotransmitter systems. This interaction can help stabilize mood and reduce withdrawal symptoms, making it a valuable tool in managing opioid addiction.
Knowing how buprenorphine affects the brain and nervous system is essential for appreciating its therapeutic benefits and potential side effects, helping patients and healthcare providers optimize treatment strategies and improve outcomes.
Stabilizing neurotransmission
Buprenorphine helps restore balance in neurotransmitter activity disrupted by chronic opioid use. By partially activating opioid receptors, it can normalize dopamine and endorphin signaling in the brain. This stabilization is crucial for managing addiction, as it helps reduce emotional fluctuations and anxiety commonly associated with withdrawal.
The partial engagement of these receptors aids in managing mood fluctuations, providing a sense of normalcy to individuals recovering from opioid addiction. This effect is essential, as it helps maintain emotional stability and supports long-term recovery efforts.
Reducing cravings and withdrawal
Buprenorphine plays a significant role in minimizing cravings and physical withdrawal symptoms. By occupying opioid receptors, it suppresses opioid withdrawal signs and reduces the severity of withdrawal symptoms and the risk of relapse. This receptor occupancy helps individuals focus on their recovery without being overwhelmed by cravings.
The use of buprenorphine containing medications in suboxone treatment provides a smoother transition away from more potent opioids, reducing the intense discomfort of withdrawal for patients receiving buprenorphine. This approach supports adherence to addiction treatment plans and enhances the likelihood of successful recovery through chronic buprenorphine treatment, buprenorphine solution, and administration buprenorphine.
Buprenorphine formulations and their impact on absorption
Different formulations of buprenorphine significantly affect its absorption, onset, and duration. Sublingual tablets and films, such as suboxone tablets and naloxone sublingual film, offer immediate efficacy by bypassing extensive first-pass metabolism, enhancing bioavailability. Extended-release formulations like Sublocade provide a sustained release, reducing the need for daily dosing.
Knowing these formulations helps patients and healthcare providers select the most suitable option based on individual needs and treatment goals, impacting the effectiveness and convenience of opioid analgesics in opioid addiction treatment and the management of opioid drugs.
Sublingual (Suboxone/Subutex) vs. extended-release (Sublocade)
Sublingual formulations, such as Suboxone pills and Subutex, have the following characteristics:
- Taken daily
- Provide immediate effects by dissolving under the tongue
- Combine buprenorphine sublingual tablets with naloxone sublingual tablet to deter misuse
- Offer a balance between effectiveness and safety in naloxone sublingual tablets therapy for sublingual tablets patients, including buprenorphine sublingual solutions.
Sublocade, an extended-release injectable, offers a simplified dosing strategy and stands out among suboxone alternatives for patients seeking less frequent administration.
- Provides a consistent release of buprenorphine over a month.
- Monthly administration by healthcare professionals reduces the daily medication burden.
- Supports adherence to treatment plans.
- Particularly beneficial for patients who may struggle with daily dosing.
- Offers a more convenient and effective treatment approach.
Bioavailability and peak plasma concentration
The bioavailability of sublingual buprenorphine is significantly higher compared to oral administration, leading to quicker peak plasma concentrations. Sublingual forms reach peak plasma concentrations approximately 60 minutes after administration, providing timely relief from withdrawal symptoms.
Knowing these metrics is crucial for optimizing dosing schedules and ensuring effective treatment. Higher bioavailability and quicker onset of effects can enhance the therapeutic benefits of buprenorphine, making it a reliable option for managing opioid dependence, potentially greater relative bioavailability.
Common physical and psychological effects of buprenorphine
Buprenorphine provides significant therapeutic benefits, including relief from withdrawal symptoms and improved mood. However, like all medications, it can also cause side effects. Knowing both the beneficial and adverse effects is essential for managing treatment effectively.
Patients and healthcare providers must be aware of these effects to optimize treatment outcomes and address any issues that may arise during therapy. This awareness can enhance adherence to treatment plans and improve overall recovery experiences.
Therapeutic effects
The therapeutic effects of buprenorphine include relief from withdrawal symptoms, stabilization of mood, and restoration of normal function. These benefits are crucial for individuals recovering from opioid addiction, as they help maintain emotional and physical stability.
By providing consistent and effective management of withdrawal symptoms, buprenorphine supports long-term recovery and enhances the quality of life for patients. This therapeutic profile makes it a valuable tool in the fight against opioid addiction.
Side effects and considerations
Common side effects of buprenorphine include constipation, headache, and sleep disturbances. These side effects are generally related to its action on opioid receptors and can often be managed with proper medical guidance. For instance, constipation may require dietary adjustments or laxatives for relief.
Other side effects, such as nausea, drowsiness, and dizziness, typically diminish as the body adjusts to the medication. Knowing these potential adverse reaction rates observed and how to manage them helps patients navigate their treatment more comfortably and effectively.
Factors that influence how buprenorphine works in the body
Several factors can influence the effectiveness and safety of buprenorphine, including liver function and genetic makeup. These individual variables can significantly alter how the body metabolizes and responds to the medication, impacting treatment outcomes.
Knowing these factors is crucial for tailoring treatment plans to individual needs, enhancing the effectiveness of buprenorphine therapy and minimizing the risk of adverse effects.
Liver function and genetics
Liver function plays a significant role in the metabolism of buprenorphine, as the drug is primarily processed in the liver. Individuals with normal hepatic function, those with impaired hepatic function, those with moderate hepatic impairment, and individuals with severe hepatic impairment may experience altered drug clearance and increased risk of side effects, necessitating dose adjustments. Liver function tests are essential for monitoring these conditions.
Genetic variations in liver enzyme activity, particularly cytochrome P450 enzymes, can also affect how different individuals metabolize buprenorphine. Knowing these genetic factors can guide personalized therapy and improve treatment outcomes.
Drug interactions
Drug interactions can significantly impact the efficacy and safety of buprenorphine, including significant pharmacokinetic interactions. For instance, medications that inhibit the CYP3A4 enzyme can increase buprenorphine levels, raising the risk of adverse effects. Conversely, drugs like rifampin that induce CYP3A4 can reduce buprenorphine’s effectiveness by lowering its blood levels.
Combining buprenorphine with substances like benzodiazepines or alcohol can lead to severe respiratory depression and increase the risk of overdose. Knowing these interactions is essential for managing buprenorphine therapy safely and effectively.
Can buprenorphine build up in the body over time?
Buprenorphine can accumulate in the body, particularly when taken consistently at prescribed doses. This accumulation is due to its long half-life and the slow process of reaching a steady-state concentration in the body.
Knowing about this buildup is crucial for managing long-term treatment and avoiding potential complications associated with drug accumulation, highlighting the importance of adhering to the prescribed dosing regimen to elevate cerebrospinal fluid pressure.
Steady-state concentration and dosing
Steady-state concentration is achieved when the rate of drug intake equals the rate of elimination, resulting in consistent drug levels in the body. This steady state is typically reached with daily dosing of buprenorphine, which is essential for maintaining effective treatment.
Achieving steady-state concentrations helps stabilize drug levels, enhancing the therapeutic benefits of buprenorphine and supporting long-term recovery. This understanding can guide dosing regimens and improve treatment outcomes.
Tolerance and dependency
Long-term use of buprenorphine can lead to tolerance, where higher doses are required to achieve the same effects. This tolerance is a common aspect of opioid use disorder therapy and needs to be managed carefully to avoid potential complications.
Physical dependence on buprenorphine can also develop, leading to withdrawal symptoms if the medication is abruptly discontinued. Differentiating between physical dependence and addiction is crucial, and managing dependence often involves a gradual tapering process to minimize withdrawal symptoms.
Bottom Line: How does buprenorphine work in the body?
Buprenorphine is a cornerstone in the treatment of opioid addiction, offering a unique combination of effectiveness and safety. Its partial agonist nature, high receptor affinity, and ceiling effect make it a valuable tool for managing opioid dependence and reducing the risk of overdose. Understanding its pharmacokinetics, mechanisms of action, and potential side effects is crucial for optimizing treatment strategies and improving patient outcomes.
By providing comprehensive insights into buprenorphine’s role in opioid addiction treatment, this guide aims to empower patients and healthcare providers with the knowledge needed to navigate the complexities of addiction therapy. With the right information, individuals can make informed decisions about their treatment, enhancing their chances of successful recovery and a better quality of life.
FAQs about buprenorphine in the body
How long does buprenorphine stay in your system?
Buprenorphine typically remains detectable in your system for 7 to 10 days, although its effects can last between 24 to 60 hours. Individual metabolism and dosage are important factors influencing these durations.
What is the ceiling effect of buprenorphine?
The ceiling effect of buprenorphine indicates that after a certain dosage, further increases do not enhance its effects, thereby significantly diminishing the risk of overdose.
How does buprenorphine compare to methadone?
Buprenorphine is safer than methadone due to its lower overdose risk and suitability for outpatient prescriptions, while methadone has stronger effects but a higher potential for overdose.
Can buprenorphine block the effects of other opioids?
Yes, buprenorphine can block the effects of other opioids due to its high affinity for opioid receptors, preventing full agonists from producing their effects.
What are the common side effects of buprenorphine?
Common side effects of buprenorphine include constipation, headache, sleep disturbances, nausea, drowsiness, and dizziness. It is important to monitor these effects and consult a healthcare provider if they persist.