Looking for suboxone alternatives? You’re not alone. Many seek other treatments for opioid use disorder due to side effects, cost, or personal reasons. This article covers FDA-approved options and non-medication approaches to help you find the right fit for your recovery.
Key Takeaways
- Suboxone alternatives include various FDA-approved medications such as Methadone and Naltrexone, as well as non-medication-based therapies to tailor treatment for opioid use disorder.
- Challenges with Suboxone, including dependency risks and stigma, highlight the importance of individualized medication-assisted treatment plans for optimal recovery outcomes.
- Emerging therapies, such as Ketamine-assisted therapy, along with behavioral approaches like Cognitive Behavioral Therapy, offer additional pathways to support individuals in their recovery journey.
What are suboxone alternatives?
Suboxone, a combination of buprenorphine and naloxone, is a well-established treatment for opioid addiction that helps reduce cravings and withdrawal symptoms. However, alternatives to Suboxone and subutex exist for various reasons. Suboxone alternatives encompass other medications and therapies that can treat opioid dependence and addiction effectively.
Individuals or healthcare providers might seek these alternatives due to side effects, access issues, cost, stigma, or simply because Suboxone might not be the best fit for every patient. The objective here is to explore these alternatives, including FDA-approved medications and non-medication-based options, to provide a comprehensive view of the treatment landscape for OUD.
Why consider alternatives to suboxone?
Despite its effectiveness, Suboxone presents certain challenges:
- Some patients may develop dependency risks.
- Patients may face access limitations.
- There can be issues with insurance coverage.
- Patient preference plays a significant role; the stigma associated with Suboxone or its side effects might push individuals to seek other options.
Clinical scenarios where Suboxone might not be the ideal fit include contraindications or poor tolerance. The importance of individualized MAT plans cannot be overstated, as each patient’s journey through opioid dependence, substance use, and addiction is unique.
Considering alternatives ensures that treatment options are tailored to an individual’s specific needs, enhancing the chances of successful recovery.
FDA-approved suboxone alternatives for opioid use disorder
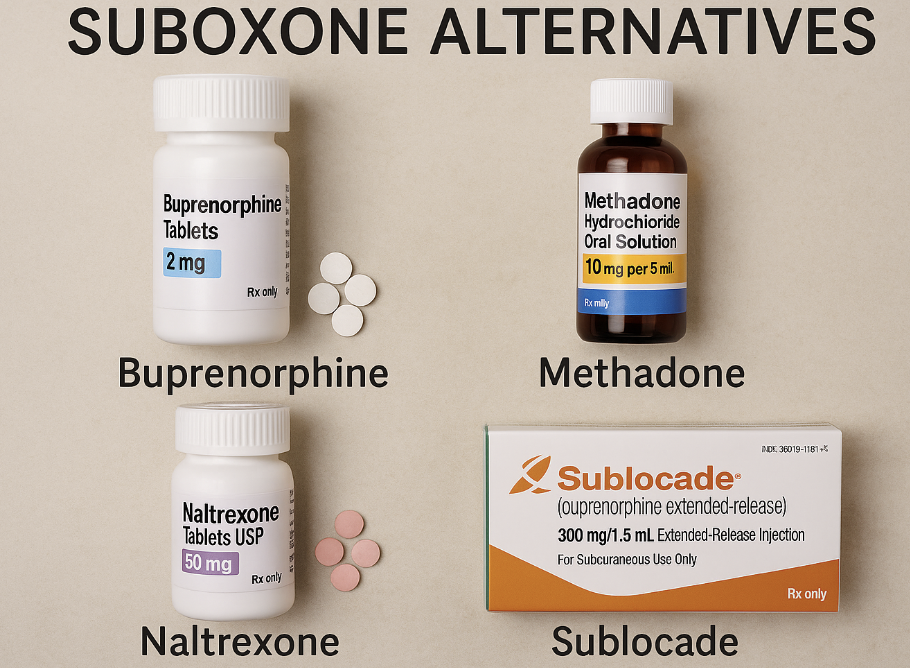
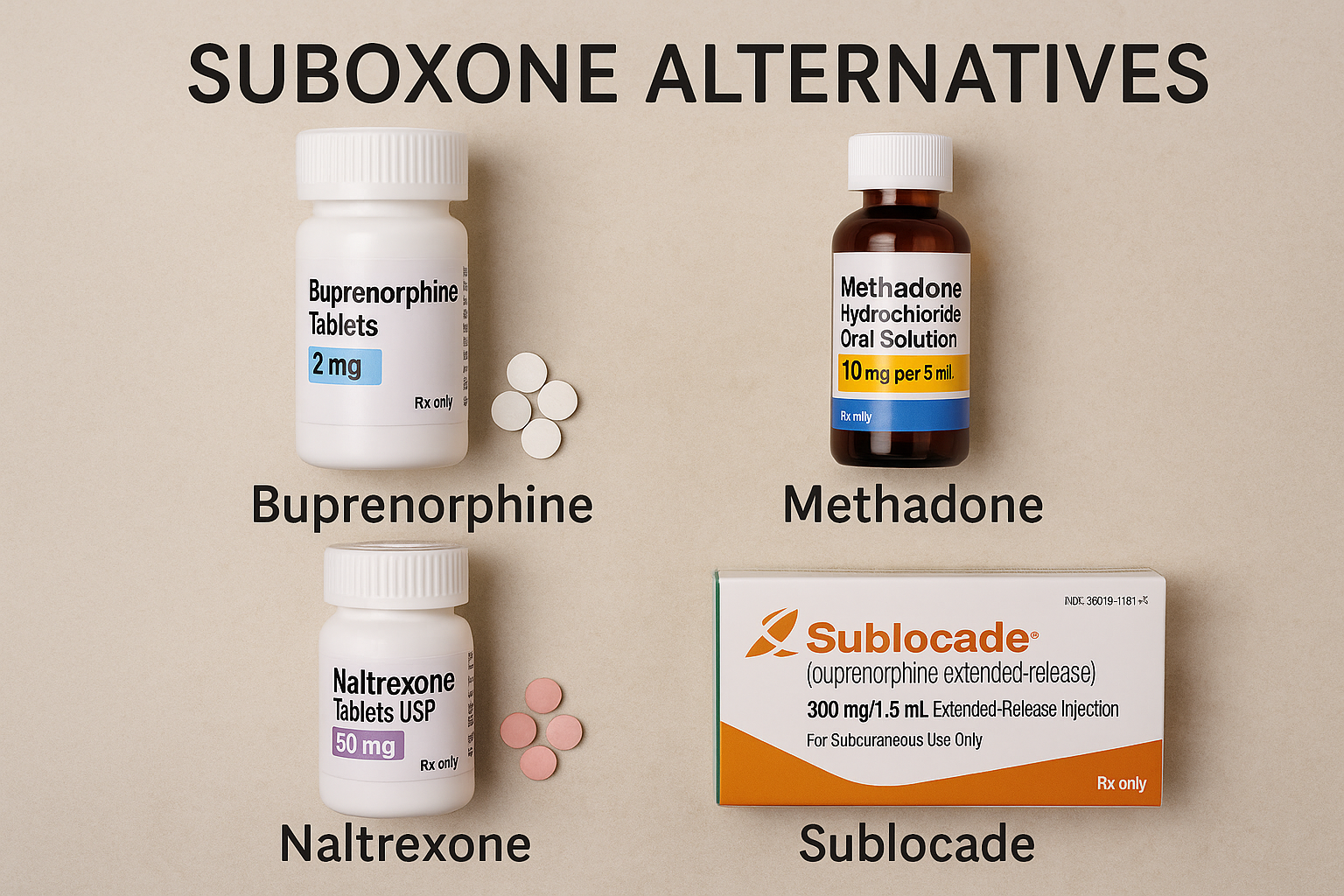
When exploring medication-assisted treatments, it’s crucial to consider FDA-approved alternatives to Suboxone. These include Methadone, Naltrexone (Vivitrol), and the Buprenorphine monoproduct, each offering distinct benefits and catering to different patient needs.
Understanding these drug formulation alternatives involves examining their mechanisms, effectiveness, and potential drawbacks. Each medication’s unique attributes can make it more suitable for specific individuals, and the following sections will delve into these different formulations details, offering a comprehensive look at each option.
Methadone
Methadone has been a cornerstone in treating opioid use disorder for over five decades, acting as a full opioid agonist by activating mu-opioid receptors in the brain. Unlike Suboxone, which is a partial agonist, Methadone’s activation is stronger. Learn more about Suboxone vs Methadone and how they compare in treatment. However, this full agonist property also means it carries a higher risk of overdose if not properly managed.
Access to methadone treatment is restricted to certified opioid treatment programs, requiring frequent visits to these facilities. Despite the initial inconvenience, regulatory changes now allow stable patients to receive up to 28 take-home doses, improving treatment compliance and continuity. The appropriate dosage is essential for effective management of their condition through methadone maintenance, as prescribed.
Methadone remains a highly effective option, particularly for those with severe opioid addiction or those who have not responded well to other treatments.
Naltrexone (Vivitrol)
Naltrexone, marketed as Vivitrol, serves as an opioid antagonist, blocking the euphoric effects of opioids and thereby helping to prevent relapse during recovery from opioid dependence. Administered as a monthly injection, it ensures sustained adherence to treatment and reduces the burden of daily medication.
However, starting Naltrexone requires a full detox to avoid precipitated withdrawal, making it less immediate than other options. Its benefits include a reduced potential for abuse and its dual role in treating both alcohol use disorder and opioid addiction. Explore a full comparison of Naltrexone vs Suboxone to better understand your options.
Common side effects like nausea and headaches can impact adherence, but its non-controlled substance status makes it a viable option for many, despite the potential for pain.
Buprenorphine monoproduct
For patients intolerant to naloxone or those who are pregnant, the only buprenorphine monoproduct offers an effective alternative to Suboxone. This medication provides similar efficacy in reducing opioid dependence and addiction, with a safety profile suitable for specific sensitive populations.
Emerging or off-label alternatives to suboxone
Beyond FDA-approved opioid medications, emerging and off-label alternatives are being explored to treat opioid dependence. These include Clonidine and Lofexidine, which help manage withdrawal symptoms, albeit not as robustly as traditional opioid treatments involving oxycodone drugs.
Ketamine-assisted therapy is another experimental approach showing promise in early-stage research. While these options are less conventional, they highlight the ongoing efforts to find diverse ways to support individuals in their recovery journey.

Clonidine and lofexidine
Clonidine and Lofexidine are primarily used for managing opioid withdrawal symptoms rather than long-term maintenance. Clonidine, though not FDA-approved for this purpose, is commonly used off-label due to its ability to reduce withdrawal symptoms.
Lofexidine, an alpha-2 adrenergic agonist approved in 2018, offers a non-opioid alternative specifically for opioid withdrawal management. It produces fewer side effects compared to Clonidine, making it a preferable choice in detox settings.
Ketamine-assisted therapy (experimental)
Ketamine-assisted therapy is under investigation for its potential to treat opioid dependence and associated mental health comorbidities. Early research suggests that Ketamine may help reduce opioid cravings and improve mood, offering a novel approach to treatment.
However, the need for more studies and controlled clinical environments is paramount to ensure safety and efficacy, especially considering the risks of ketamine addiction in unsupervised use. This experimental therapy represents a frontier in addiction treatment, highlighting the innovative efforts to address opioid addiction comprehensively.
Non-medication-based alternatives to suboxone
For those who prefer non-pharmacologic treatment options, holistic or behavioral approaches offer viable pathways to recovery at the clinic, especially when guided by a treatment team. These methods can be particularly effective when combined with medical or therapeutic oversight.
Options include:
- Cognitive Behavioral Therapy (CBT)
- Contingency management
- 12-step programs
- Peer support groups
- Structured rehab programs
Each offers unique benefits in managing opioid dependence and addiction to treat opioid addiction.

Cognitive behavioral therapy (CBT) and contingency management
Cognitive Behavioral Therapy (CBT) is a cornerstone in addiction treatment, helping individuals manage cravings and triggers by altering negative thought patterns. This therapy fosters resilience and equips patients with coping strategies essential for long-term recovery.
Contingency management complements CBT by using a reward system to reinforce sobriety goals. This combination can significantly enhance motivation and adherence to the recovery plan, making it a powerful tool in the addiction treatment arsenal.
12-step programs and peer support groups
12-step programs like Narcotics Anonymous (NA) and secular support groups provide:
- Community and accountability, essential for long-term engagement in recovery
- A supportive environment where individuals can share experiences
- Strategies for managing addiction
The sense of belonging and continuous encouragement from peers can be a powerful motivator, helping individuals stay committed to their recovery journey.
Residential rehab and intensive outpatient programs (IOP)
Residential rehab and Intensive Outpatient Programs (IOP) offer structured pathways for those seeking MAT-alternative treatments. IOPs provide:
- A minimum of nine hours of treatment per week
- Individual therapy
- Group therapy
- Family therapy
These programs allow patients to remain in their home environments.
These programs are crucial components of addiction treatment, often serving as transitions from higher levels of care. They offer integrated therapy models and medical monitoring, enhancing treatment outcomes and supporting community life adjustments.
How to choose the right alternative to suboxone
Choosing the right alternative to Suboxone involves evaluating several factors, including:
- The severity of addiction
- Co-occurring disorders
- History of relapse
- Medical history
Support systems also play a crucial role in this decision-making process.
Consulting addiction specialists or MAT providers helps ensure the chosen treatment aligns with the individual’s specific needs and health profile. A tailored approach increases the likelihood of successful recovery and long-term sustainability.
Risks and limitations of suboxone alternatives
While exploring Suboxone alternatives, it’s essential to consider their safety profiles and potential risks. Each medication and treatment option comes with its unique set of benefits and limitations.
Going off Suboxone without medical supervision can lead to severe withdrawal symptoms and increased risks of relapse. Evidence-based care remains crucial, even when opting for holistic or experimental paths.
Bottom Line: Are suboxone alternatives right for you?
Selecting the appropriate alternative to Suboxone involves understanding personal treatment needs, potential benefits, and associated risks. Each individual’s journey is unique, and what works for one person might not be suitable for another.
Consulting with addiction specialists and doctors provides tailored insights into whether alternatives may be suitable based on personal health profiles. Ultimately, personalized, medically guided addiction care is paramount for successful recovery.
FAQs about suboxone alternatives
What are the main FDA-approved alternatives to Suboxone?
The primary FDA-approved alternatives to Suboxone are Methadone, Naltrexone (Vivitrol), and Buprenorphine monoproduct. Each of these options provides different approaches to addiction treatment.
Why might someone seek alternatives to Suboxone?
Individuals may seek alternatives to Suboxone primarily due to side effects, accessibility challenges, financial considerations, stigma, or the belief that it may not be the most suitable treatment for their specific needs.
How does Methadone compare to Suboxone in treating opioid dependence?
Methadone, being a full opioid agonist, offers strong relief from cravings and withdrawal but necessitates daily clinic visits initially. In contrast, Suboxone is a partial agonist with a reduced risk of misuse, making it a more flexible option for some patients in treating opioid dependence.
What are some experimental alternatives to Suboxone?
Experimental alternatives to Suboxone include Clonidine and Lofexidine for managing withdrawal symptoms, as well as Ketamine-assisted therapy, which remains under investigation. These alternatives offer potential pathways for treatment in opioid dependency.
Can non-medication-based treatments be effective for opioid dependence?
Non-medication-based treatments, such as cognitive behavioral therapy, contingency management, and structured rehabilitation programs, can be effective for opioid dependence, particularly when utilized alongside medical oversight. Therefore, integrating these therapies into treatment plans may enhance recovery outcomes.