Buprenorphine is a medication primarily used to treat opioid addiction. It helps reduce cravings and withdrawal symptoms, making it easier for individuals to focus on recovery. In this article, we will explore what buprenorphine is, how it works, its benefits, medical uses, side effects, and comparisons with other opioid addiction treatments.
Key Takeaways
- Buprenorphine, classified as a Schedule III controlled substance, is primarily used for treating opioid addiction and shows a unique mechanism as a partial agonist, reducing cravings and withdrawal symptoms without producing intense euphoria.
- The medication features a ceiling effect, limiting the risk of overdose and allowing for flexible dosing schedules, which contribute to its effectiveness and safety in Opioid Use Disorder (OUD) treatment.
- Buprenorphine is accessible through certified healthcare providers, offering various formulations that enhance patient adherence and support a comprehensive approach to recovery when combined with counseling and behavioral therapies.
Buprenorphine definition and classification
Buprenorphine is a medication used primarily in the treatment of opioid addiction and dependence. It belongs to a class of drugs known as opioid partial agonists, which means it binds to the same receptors in the brain as other opioids but produces a milder effect.
Unlike full opioid agonists, such as heroin and methadone, which fully activate the opioid receptors and produce a significant euphoric effect, the opioid partial agonist buprenorphine only partially activates these receptors. This unique property allows buprenorphine to reduce cravings and opioid withdrawal symptoms without producing the intense highs associated with full agonists, making it a safer option for long-acting opioid use.
Buprenorphine is classified as a Schedule III controlled substance under the U.S. DEA regulations—similar to Suboxone, prompting the question, is Suboxone a controlled substance, and what implications does that have for its prescription and use. This classification indicates that while the drug has a potential for abuse, it is lower compared to Schedule I or II substances, and it has accepted medical uses. This classification also means that healthcare providers must follow specific guidelines when prescribing buprenorphine, ensuring it is used safely and effectively.
In summary, buprenorphine’s classification and mechanism of action make it a powerful tool in the treatment of opioid addiction, offering a balance of efficacy and safety that is crucial for patients battling this challenging condition.
How buprenorphine works in the body
Buprenorphine works by interacting with opioid receptors in the brain, particularly the mu-opioid receptor, which plays a significant role in pain perception and addiction. Buprenorphine affects pain signals and alleviates discomfort to treat pain by binding to these receptors, which can reduce anxiety and stress related to pain.
One of the key benefits of buprenorphine treatment is its ceiling effect, which limits the extent of euphoria and respiratory depression. This means that after a certain dose, taking more buprenorphine will not increase its effects, reducing the risk of overdose. This ceiling effect is a crucial safety feature, especially for patients receiving buprenorphine who might be at risk of relapse.
Buprenorphine has a long half-life, which allows for flexible dosing schedules, including a dose of buprenorphine or even alternate-day dosing. This extended duration of action helps maintain stable levels of the medication in the bloodstream, ensuring consistent therapeutic effects and making it easier for patients to adhere to their treatment regimen.
Overall, the unique pharmacological properties of buprenorphine make it an effective and safer option for treating opioid dependence, providing patients with a reliable means to manage their addiction and improve their quality of life.
Medical uses of buprenorphine
The primary medical use of buprenorphine is in Medication-Assisted Treatment (MAT) for opioid use disorder (OUD). MAT combines medications with counseling and behavioral therapies to provide a comprehensive approach to treating substance use disorders. Buprenorphine helps reduce cravings and withdrawal symptoms, making it easier for patients to focus on their recovery and engage in therapy.
In addition to its use in treating opioid addiction, buprenorphine is also used for pain management, particularly for chronic pain when other pain relief methods are ineffective. It provides effective pain relief with a lower risk of abuse compared to other opioids, making it a valuable option for patients with chronic pain.
There are several FDA-approved buprenorphine products available for different uses. For opioid use disorder, options include Suboxone, Subutex, Sublocade, Zubsolv, and Probuphine. For pain management, Butrans and Belbuca are commonly prescribed. These formulations offer various methods of administration, allowing healthcare providers to tailor treatment to the specific needs of each patient, including the use of opioid medicine and opioid medication.
Benefits of using buprenorphine for opioid addiction treatment
Buprenorphine treatment offers several significant benefits for individuals struggling with opioid addiction. One of the primary advantages is its ability to reduce opioid cravings and withdrawal symptoms, which are major barriers to recovery. By alleviating these symptoms, buprenorphine helps patients maintain their focus on recovery and reduces the likelihood of relapse.
Another key benefit is that buprenorphine allows for stable maintenance therapy without causing intense sedation. This enables patients to lead more normal lives, engage in daily activities, and participate in therapy sessions without the debilitating effects of sedation. Additionally, buprenorphine is safer than methadone in outpatient settings, as it carries a lower risk of overdose and can be prescribed by certified providers in an office setting.
Buprenorphine can be prescribed in-office by certified providers who have obtained a DATA 2000 waiver, making it more accessible for patients compared to methadone, which typically requires visits to a specialized clinic. This accessibility is crucial for ensuring that more individuals can receive the treatment they need without the added burden of frequent clinic visits. Additionally, some healthcare providers may choose to prescribe methadone as part of a comprehensive treatment plan.

Side effects and risks of buprenorphine
Like all medications, buprenorphine treatment comes with potential side effects and risks. Common side effects include:
- headache
- nausea
- constipation
- sweating
- insomnia
While these side effects are generally mild and manageable, they can cause discomfort for some patients.
More serious but rare risks include respiratory depression, adverse effects, and liver function issues, including fatal respiratory depression and adverse drug reactions. These risks highlight the importance of careful monitoring by healthcare providers, especially during the initial phases of treatment or when adjusting doses. Patients should be informed about these potential risks and advised to seek medical attention if they experience any concerning symptoms.
There is also a risk of diversion and misuse of buprenorphine, although this risk is lower compared to full agonists like heroin or methadone, and is especially relevant in discussions around Suboxone addiction. Healthcare providers mitigate this risk by administering buprenorphine according to strict prescribing guidelines and closely monitoring patients for signs of substance abuse, drug abuse, physical dependence, and other medicines.
Additionally, combining buprenorphine naloxone with formulations like Suboxone can help reduce the potential for misuse by causing withdrawal symptoms if the medication is injected.
Buprenorphine vs. other medications for OUD
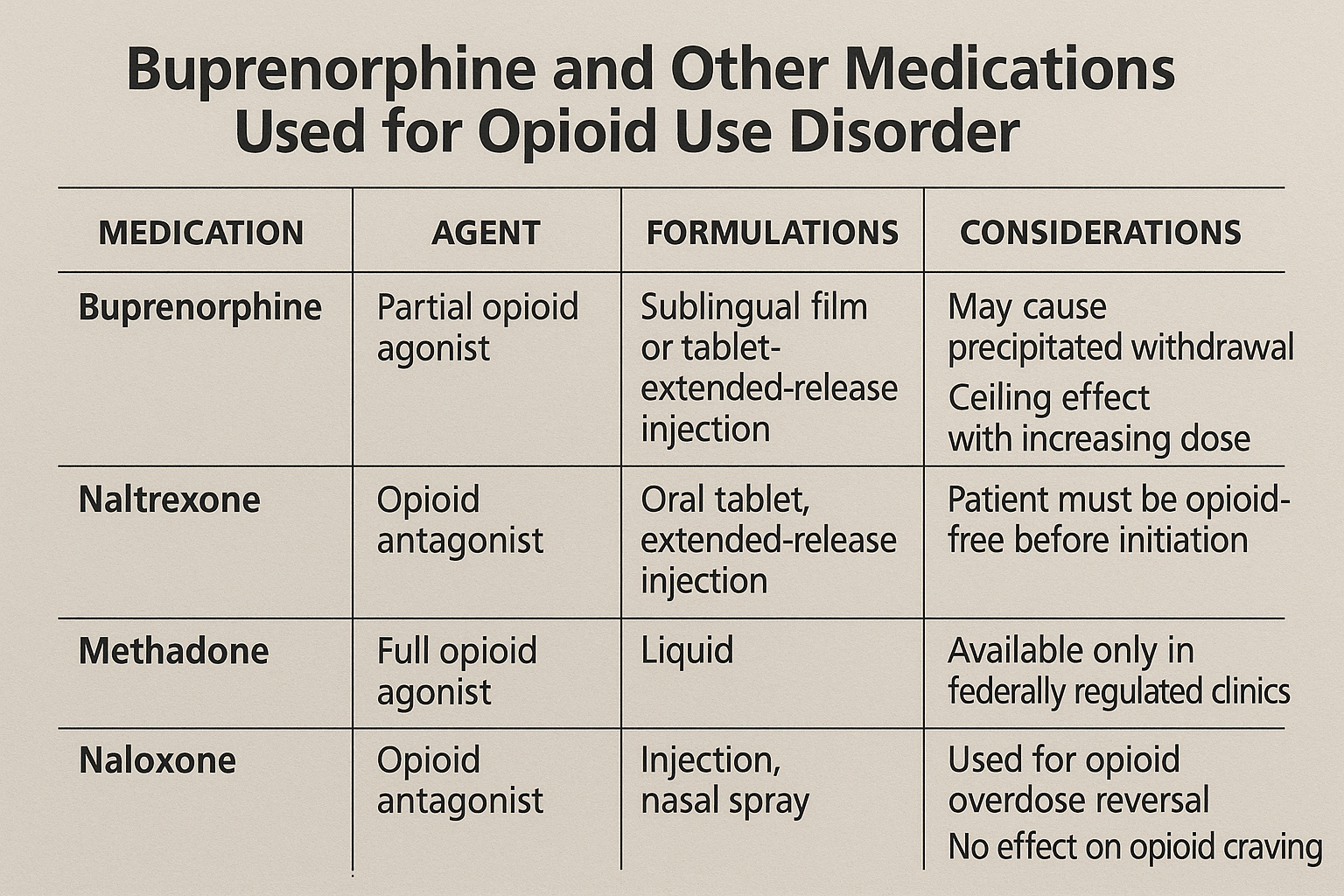
When it comes to treating opioid use disorder, buprenorphine is often compared to other medications like methadone and naltrexone. Methadone is characterized by several properties, which are directly compared with buprenorphine in this detailed Suboxone vs methadone guide, including its full agonist action, daily clinic visits, and higher overdose risk.
- Being a full opioid agonist that fully activates the opioid receptors
- Providing effective relief from withdrawal symptoms and cravings
- Having a higher risk of overdose and sedation
- Usually requiring daily visits to a methadone clinic, which can be a barrier for some patients.
Naltrexone, on the other hand, is an opioid antagonist that blocks the effects of opioids without activating the receptors. This means that patients must be fully detoxed before starting naltrexone, which can be a significant hurdle. Naltrexone is suitable for patients who have already completed detox and are motivated to stay opioid-free. You can learn more about how these treatments compare in Naltrexone vs Suboxone. Opioid antagonists like naltrexone play a crucial role in treatment.
Buprenorphine’s partial agonist properties offer a balance between both buprenorphine, providing effective relief from withdrawal symptoms while reducing the risk of overdose. It can be prescribed in-office, allowing for greater accessibility and convenience for patients. Ultimately, the choice between these medications depends on the individual patient’s needs, preferences, and medical history.
How to take buprenorphine: Methods and formulations
Buprenorphine is available in several formulations, each offering different methods of administration to suit various patient needs. Common formulations include sublingual films and tablets, injections like Sublocade and buprenorphine extended release injection, and implants such as Probuphine. These options allow healthcare providers to tailor treatment to the specific requirements and preferences of each patient.
Different dosing options include:
- Daily dosing with sublingual tablets and films.
- Monthly injections like Sublocade, which provide a longer-lasting option that can improve adherence.
- Implants such as Probuphine, offering sustained release of the medication over several months, reduce the need for frequent dosing with a sublingual tablet and various dosage forms.
When taking buprenorphine sublingually, it is essential to follow special instructions:
- Avoid eating before taking the dose.
- Avoid drinking before taking the dose.
- Avoid eating after taking the dose.
- Avoid drinking after taking the dose.
Following these guidelines helps maximize the medication’s effectiveness and ensures patients receive the full therapeutic benefits.
Who can and cannot take buprenorphine?
Buprenorphine treatment is indicated for adults with moderate to severe opioid use disorder, providing a valuable tool in the fight against addiction. However, certain contraindications and precautions must be considered to ensure the safety and effectiveness of the treatment.
Pregnant women can safely take buprenorphine, as studies have shown it to be effective in reducing opioid use and improving outcomes for both the mother and the baby, including the prevention of neonatal abstinence syndrome and neonatal opioid withdrawal syndrome. Adolescents may also benefit from buprenorphine treatment, although careful monitoring and appropriate dosing are essential.
Patients with liver disease require special consideration, as buprenorphine can affect liver function. Healthcare providers must carefully assess the patient’s liver health and adjust the treatment plan accordingly to minimize risks. Overall, a thorough evaluation by a qualified provider is crucial to determine if buprenorphine is the right choice for each individual patient.
How effective is buprenorphine in recovery programs?
Buprenorphine maintenance has been shown to significantly improve retention in treatment programs for opioid use disorder, especially at higher doses. Clinical trials have demonstrated that buprenorphine is more effective than a placebo in maintaining treatment adherence, making it a valuable tool in recovery programs.
The effectiveness of buprenorphine is often influenced by the dosage, with higher doses leading to better outcomes in terms of retention and abstinence. Studies have found that although buprenorphine generally has lower retention rates compared to methadone, the abstinence outcomes are similar.
Additionally, buprenorphine’s ability to facilitate easier initiation of treatment compared to naltrexone, which requires complete withdrawal before administration, contributes to its effectiveness. Despite its benefits, research highlights a concerning dropout rate from buprenorphine treatment, with over 50% of patients failing to remain in treatment after six months.
Integrating therapy and counseling with buprenorphine treatment can help improve these outcomes and support long-term recovery.
Misconceptions and stigma around buprenorphine
Buprenorphine treatment is often surrounded by misconceptions and stigma, which can deter individuals from seeking this life-saving medication. One common myth is that taking buprenorphine is simply replacing one drug with another. In reality, buprenorphine is a medically supervised treatment that helps manage opioid dependence and supports recovery.
Another misconception is that individuals taking buprenorphine are not truly sober. This stigma undermines the effectiveness of buprenorphine as a legitimate medical treatment and can discourage patients from adhering to their treatment plans. It is essential to emphasize that buprenorphine is a medication, not a crutch, and it plays a critical role in helping individuals achieve and maintain sobriety.
Addressing these misconceptions with supportive, evidence-based rebuttals can help reduce stigma and encourage more individuals to seek the treatment they need. By promoting a better understanding of buprenorphine, we can support those on their journey to recovery and improve overall public health.
How to access buprenorphine treatment
Accessing buprenorphine treatment involves several steps:
- Finding a qualified provider.
- Certified healthcare providers who have obtained a DATA 2000 waiver can prescribe buprenorphine, making it more accessible to patients.
- Utilizing telehealth services, which have expanded access by allowing patients to receive prescriptions and follow-up care remotely.
Once a provider is found, the next step is getting a prescription. Patients should discuss their medical history and treatment goals with their provider to determine the appropriate dosage and formulation. Insurance coverage and cost considerations are important factors to address, as buprenorphine treatment can be expensive without coverage. Many insurance plans, including Medicaid, cover buprenorphine treatment, and there are federally funded programs available to assist those in need.
Local MAT access support programs can also provide resources and guidance to help individuals start and maintain their buprenorphine treatment. By navigating these steps and accessing available resources, patients can embark on their journey to recovery with the support they need.

Alternatives to buprenorphine for opioid treatment
While buprenorphine is a highly effective treatment for opioid addiction, it is not the only option available. Methadone is another widely used medication with the following characteristics:
- Acts as a full opioid agonist, fully activating opioid receptors to alleviate withdrawal symptoms and cravings.
- Typically administered in a specialized clinic setting.
- Requires daily visits, which can be a barrier for some patients.
Naltrexone (marketed as Vivitrol) is an opioid antagonist that works by blocking the effects of opioids without activating the receptors. However, patients must be fully detoxed before starting naltrexone, which can be a significant hurdle. Naltrexone is particularly suitable for patients who have already completed detox and are highly motivated to stay opioid-free.
Non-medication-based treatments, such as behavioral therapy and counseling, are also important components of a comprehensive treatment of opioid dependence for opioid use disorder. While these therapies alone may not be sufficient for many individuals, they play a crucial role in supporting long-term recovery when combined with medications like buprenorphine or methadone. Each treatment option has its advantages and limitations, and the best choice depends on how to treat opioid addiction based on the individual needs and circumstances of the patient.
Bottom Line: Is buprenorphine right for you or your loved one?
Deciding whether buprenorphine treatment is the right choice for you or your loved one involves considering various factors, including the severity of opioid dependence, medical history, and personal preferences. Buprenorphine has proven to be an effective and accessible option for many individuals struggling with opioid addiction, offering a safer alternative to full opioid agonists and the flexibility of office-based treatment.
It is essential to seek a professional evaluation from a qualified healthcare provider who can assess your specific situation and recommend the most appropriate treatment plan. Buprenorphine treatment, combined with counseling and behavioral therapies, provides a comprehensive approach to managing opioid use disorder and supporting long-term recovery.
If you or your loved one is struggling with opioid addiction or opioid dependency, do not hesitate to reach out to a healthcare provider for help. With the right support and treatment, recovery is possible, and buprenorphine can be a vital part of that journey.
FAQs about buprenorphine
Can you get high from buprenorphine?
Buprenorphine does produce some euphoric effects, but its status as a partial opioid agonist and its ceiling effect significantly limit the potential for getting high. This makes buprenorphine a safer alternative for treating opioid dependence.
Is it safe to take buprenorphine long-term?
Buprenorphine is considered safe for long-term use of buprenorphine when prescribed by a healthcare provider. It effectively manages opioid dependence, aiding in patient recovery and stability.
How does buprenorphine affect pregnancy?
Buprenorphine can be safely used during pregnancy to treat opioid dependence and has been shown to improve outcomes for both mother and baby. Close monitoring by a healthcare provider is essential for pregnant women using this medication.
What’s the difference between Suboxone and buprenorphine?
Suboxone is a combination of buprenorphine and naloxone, specifically formulated to minimize misuse risks, while buprenorphine can be used independently for treating opioid dependence. The inclusion of naloxone in Suboxone enhances safety by preventing injection misuse.
Can you overdose on buprenorphine?
Yes, it is possible to overdose on buprenorphine, particularly when combined with other central nervous system depressants. Adhering strictly to the prescribed dosage by a healthcare provider is crucial to minimize this risk.
















