When it comes to treating opioid addiction, the choice between Suboxone versus Methadone can be crucial. Suboxone offers flexibility and a lower risk of overdose, while Methadone provides robust support for severe cases. In this article, we’ll explore the key differences, effectiveness, side effects, and other factors to help you make an informed decision.
Key Takeaways
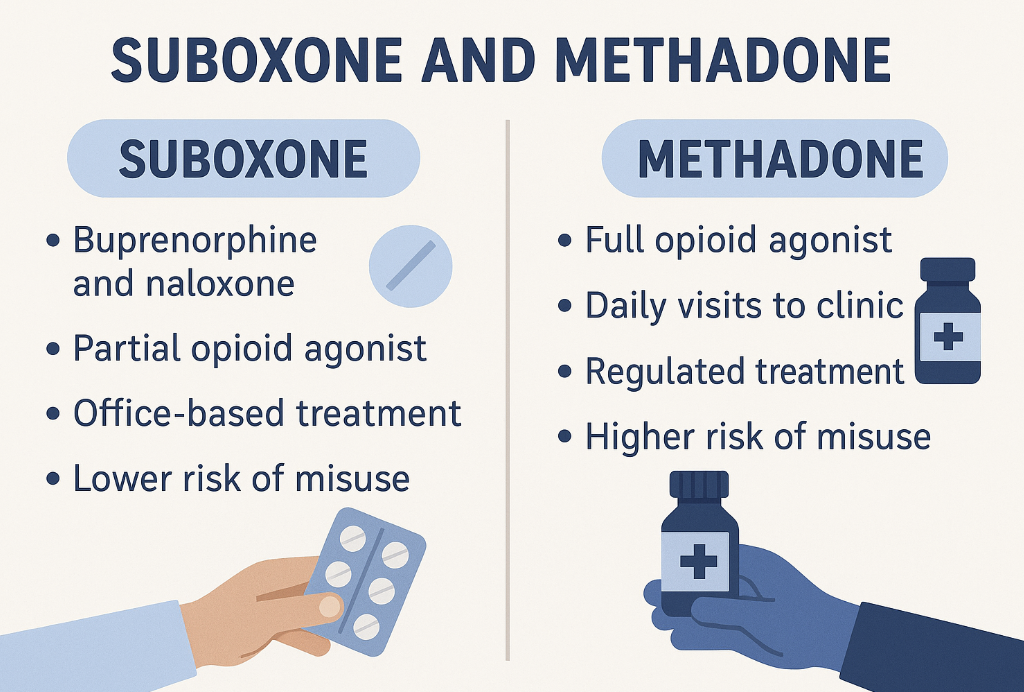
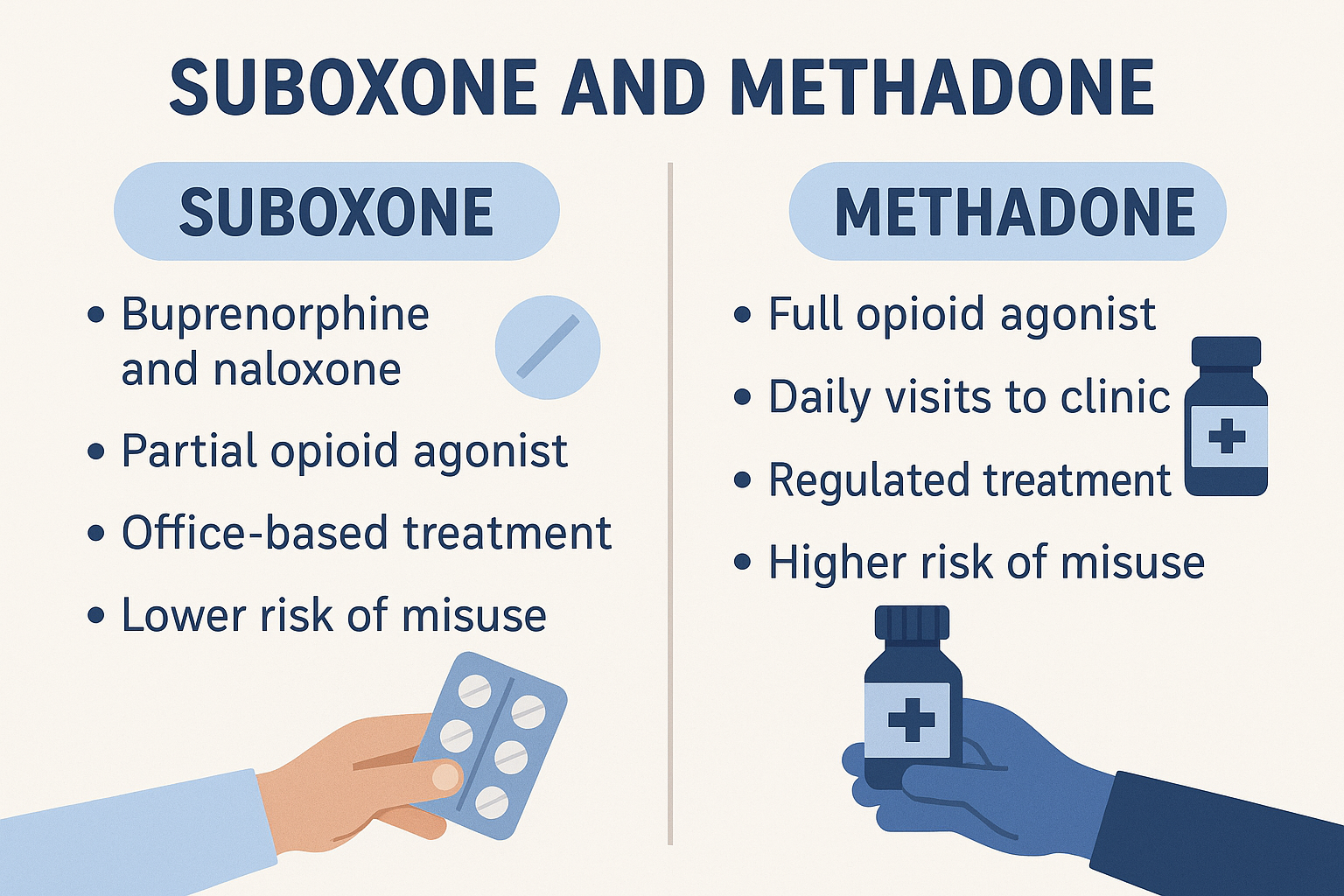
- Suboxone is a partial agonist and safer in terms of overdose risk, making it suitable for flexible outpatient treatment, while Methadone is a full agonist indicated for severe opioid dependence requiring structured support.
- Methadone is dispensed in highly regulated clinics, necessitating daily visits, which can pose accessibility challenges, whereas Suboxone can be prescribed by various healthcare providers and filled at regular pharmacies.
- Both medications effectively reduce opioid cravings, but the choice between Suboxone and Methadone should be tailored to individual patient needs, considering factors like addiction severity, treatment history, and personal support systems.
Suboxone vs Methadone: Quick Comparison for Immediate Clarity
To start, here’s a quick glance comparison table to highlight the key differences and similarities between Suboxone and Methadone:
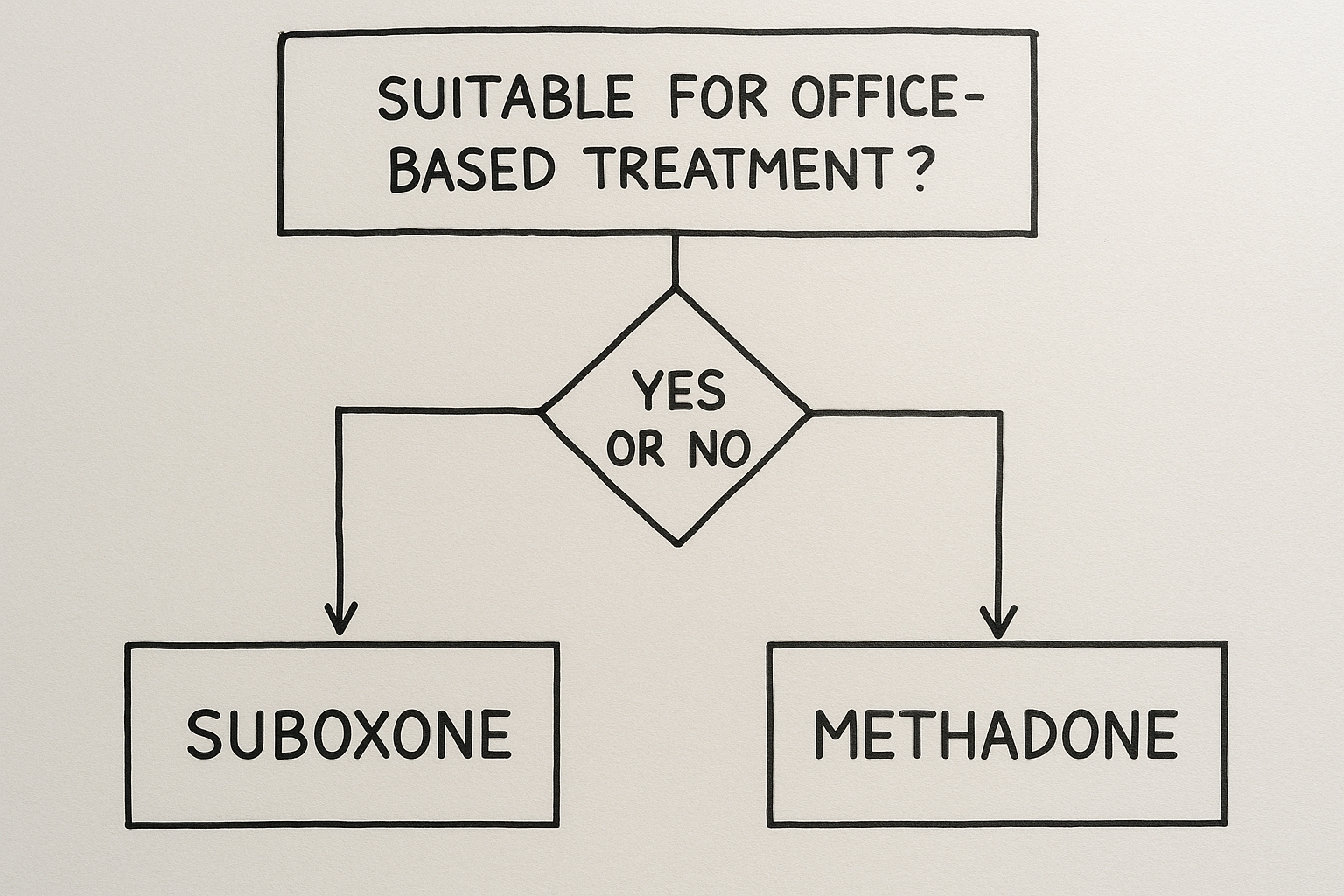
Which is better for whom? Suboxone might be the preferred choice for those seeking outpatient ease and flexibility, while Methadone could be more suitable for individuals with severe or long-term opioid dependence. Methadone’s daily clinic visits provide a structured support system that some patients may find beneficial, though others might consider it inconvenient.
In Short:
- Accessibility: Suboxone is more accessible due to fewer regulatory restrictions, unlike Methadone, which requires daily visits to specialized clinics.
- Regulations: Methadone is highly regulated and dispensed only in approved clinics.
- Overdose Potential: Suboxone has a lower risk of overdose due to its ceiling effect, unlike Methadone, which carries a higher risk.
What Is Suboxone? Understanding the Components and Purpose
Suboxone is a combination medication. It is used to treat opioid addiction. It comprises two active ingredients: buprenorphine and naloxone. Buprenorphine is a partial opioid agonist, meaning it partially activates the brain’s opioid receptors, which helps to reduce cravings and withdrawal symptoms without producing the intense euphoric effects of full agonists like heroin or methadone. Naloxone, on the other hand, is an opioid antagonist that blocks opioid effects and is included to deter misuse, as it can precipitate withdrawal symptoms if injected.
Suboxone is FDA-approved for opioid use disorder (OUD) and is typically administered as a sublingual film or tablet that dissolves under the tongue. This method ensures that the medication is absorbed effectively, providing relief from opioid cravings and withdrawal symptoms.
Combining these two components, Suboxone offers a safer and more manageable option for many individuals seeking recovery.
What Is Methadone? A Full Agonist with a Long Track Record
Methadone is a full opioid agonist that has been used for decades to treat opioid addiction. Unlike partial agonists, Methadone fully activates the brain’s opioid receptors, effectively reducing cravings and withdrawal symptoms. This makes it particularly effective for individuals with severe or long-term opioid dependence, providing a stable and controlled way to manage their addiction.
Methadone is dispensed through opioid treatment programs (OTPs), which are tightly regulated to ensure safe and effective use. Patients must visit these clinics daily to receive their doses, which allows for close monitoring that is carefully monitored and adjustment of the medication as needed.
Methadone’s long track record of success and its ability to handle more complex cases of addiction make it a valuable option in the arsenal of addiction medicine.
Suboxone vs Methadone: Mechanism of Action Compared
Suboxone and Methadone both target the brain’s opioid receptors but do so in fundamentally different ways. Suboxone, with its partial agonist buprenorphine, only partially activates these receptors, providing enough stimulation to reduce cravings and withdrawal symptoms without the full euphoric effect. This partial activation also results in a “ceiling effect,” where increasing the dose beyond a certain point does not enhance its effects, making it safer in terms of overdose risk.
Methadone, as a full agonist, fully activates the opioid receptors, providing a linear response to increasing doses. This means that higher doses can produce stronger effects, which can be beneficial for managing severe addiction but also increases the risk of methadone overdose and respiratory depression. The pharmacological differences between these medications significantly impact their safety profiles and potential for misuse.
Suboxone’s ceiling effect not only makes it safer but also reduces the severity of withdrawal symptoms, supporting a more manageable Suboxone detox process, aiding in reducing withdrawal symptoms compared to Methadone. This makes Suboxone a more stable therapeutic option for many patients, as it minimizes the risk of misuse and respiratory issues. These differences underscore the importance of selecting the right medication based on individual needs and circumstances.
Effectiveness of Suboxone vs Methadone in Treating Opioid Addiction
Both Suboxone and Methadone have proven effective in reducing opioid cravings and usage, but their effectiveness can vary based on individual patient needs. Methadone’s full agonist properties make it more suitable for individuals with severe opioid dependence, providing robust and consistent relief from cravings and withdrawal symptoms. This effectiveness is often reflected in higher patient retention rates within Methadone treatment programs.
Suboxone, with its lower risk of overdose due to the ceiling effect, offers a safer alternative for many patients, particularly those who require a more flexible suboxone treatment option. Its ability to be prescribed outside of specialized clinics makes it accessible to a broader population, allowing patients to integrate treatment more seamlessly into their daily lives.
Both medications are powerful tools in the fight against opioid addiction, and their success often depends on matching the right treatment to the patient’s specific situation, as both can be equally effective.
Risks and Side Effects: Methadone vs Suboxone Safety Comparison
Methadone and Suboxone each come with their own set of risks and methadone side effects. Common side effects for Methadone include constipation, drowsiness, sweating, and dry mouth. More serious potential risks involve respiratory depression and the potential for overdose, especially if the drug is not used as prescribed. This heightened risk necessitates daily supervision and structured support through Methadone clinics.
Suboxone’s side effects are generally milder and include nausea, headache, sweating, and constipation. The inclusion of naloxone in Suboxone helps deter misuse by precipitating withdrawal symptoms if the medication is injected. One of the serious risks associated with Suboxone is precipitated withdrawals, which can occur if the medication is taken too soon after using other opioids.
However, the ceiling effect of buprenorphine makes it less likely to cause respiratory depression, offering a lower risk profile compared to Methadone. The potential for overdose is a significant concern with Methadone due to its full agonist nature, while Suboxone’s partial agonist properties provide a safer alternative for many patients. Understanding these risks and side effects is crucial in making an informed decision about which treatment is most appropriate.
Suboxone vs Methadone: Accessibility, Regulations, and Stigma
Accessibility and regulatory differences between Suboxone and Methadone play a significant role in treatment decisions. Methadone is highly regulated and can only be dispensed at certified clinics, requiring patients to visit these facilities daily for their doses. This can be a barrier for many individuals seeking treatment, especially those with limited access to transportation or who live far from a clinic.
Suboxone, on the other hand, can be prescribed by various healthcare providers and filled at regular pharmacies, making it more accessible for many patients. This flexibility allows patients to receive treatment in a more convenient and less stigmatized setting. However, the stigma associated with Methadone treatment can deter some patients from seeking help. During the COVID-19 pandemic, some regulations for Methadone were relaxed, allowing for take-home doses, which demonstrated that stricter regulations might not always be necessary.
Public perception and stigma also impact patient willingness to start treatment. Methadone clinics are often viewed negatively, and this perception can contribute to self-stigmatization and reluctance to engage with these programs. Insurance coverage for opioid use disorder treatments has improved, making it easier for patients to access medications, although some still prefer buprenorphine due to fewer restrictions.
Cost Comparison: Is Suboxone or Methadone More Affordable?
The cost of treatment can be a determining factor when choosing between Suboxone and Methadone. Suboxone typically has a higher initial cost due to the price of the medication and the need for regular physician visits, which may add to overall treatment expenses. However, its accessibility and the ability to be prescribed outside of specialized clinics can offset some of these costs for patients who cannot easily access Methadone clinics.
Methadone treatment can be more cost-effective in the long run, especially for individuals requiring longer-term care. It is often provided at certified clinic specialized clinics at lower prices, which can make it a more affordable option for some patients.
Insurance coverage for both Suboxone and Methadone varies significantly and can impact the overall affordability of each treatment option. Additionally, the total cost of treatment may include associated healthcare services, such as counseling and regular health check-ups, which can differ between Suboxone and Methadone protocols.
Which Is Right for You: Choosing Between Suboxone and Methadone
Choosing the right treatment for opioid addiction depends on individual circumstances, including the severity of dependence, treatment history, and personal support needs. Suboxone provides a flexible treatment option that can be prescribed outside of specialized clinics, making it more accessible for many patients. Its ceiling effect makes it a safer choice in terms of overdose risk, particularly for those who may struggle with suboxone addiction.
Methadone is often recommended for individuals with severe opioid addiction due to its full agonist properties and daily structured support. The daily visits to Methadone clinics provide a level of supervision and consistency that can be beneficial for those needing a more controlled environment. However, the structured nature of Methadone treatment may pose challenges for others needing flexibility.
Patient stories and sample scenarios can help guide the choice. For example, someone with a long history of opioid addiction and multiple relapses might benefit from the structured support of Methadone. In contrast, someone with a stable environment and strong support network might find Suboxone a more convenient and effective option. Consulting with a healthcare provider is essential for determining the most suitable medication-assisted treatment for opioid use disorder and addressing any underlying issues related to substance abuse.
Alternatives to Suboxone and Methadone: Exploring Other Options
While Suboxone and Methadone are the most well-known MAT options, individuals may also consider Suboxone alternatives such as Naltrexone or non-medication therapies. Naltrexone (Vivitrol) is an opioid antagonist that naloxone blocks the effects of opioids and is administered as a monthly injection. It is particularly useful for individuals who have already detoxed from opioids and are looking to prevent relapse.
Non-medication approaches, such as cognitive-behavioral therapy (CBT) and contingency management, can also be effective in treating opioid addiction and treating opioid use disorder. These therapies can be used in combination with MAT to provide a comprehensive opioid addiction treatment plan.
Understanding the full range of treatment options and when they might be preferred is crucial for individuals on their recovery journey.
Bottom Line: Suboxone vs Methadone – What’s Most Important?
At the end of the day, both Suboxone and Methadone are effective tools in the fight against opioid addiction. The best choice depends on individual needs, circumstances, and preferences. Suboxone offers flexibility and a lower risk of overdose, making it a viable option for many patients. Its ability to be prescribed outside of specialized clinics enhances accessibility, which can be a critical factor for those with limited access to healthcare facilities.
Methadone, with its full agonist properties, provides robust support for those with severe or long-term opioid dependence. The daily methadone clinic visits offer structured supervision that some patients may find beneficial.
Regardless of the medication chosen, the most important aspect is getting into treatment and starting the journey toward recovery. Resources for finding treatment providers or support networks, such as American Addiction Centers, can be invaluable, ensuring that individuals receive the help they need to overcome opioid addiction.
FAQs: Suboxone and Methadone Questions Answered
Can you switch from Methadone to Suboxone?
Yes, you can switch from Methadone to Suboxone, but it must be done carefully under a healthcare provider's supervision to prevent precipitated withdrawal, often requiring a tapering down of the Methadone dose beforehand.
Which has worse withdrawal symptoms, Suboxone or Methadone?
Methadone withdrawal is generally more prolonged and severe, often lasting up to 20 days, compared to Suboxone withdrawal, which typically lasts up to 10 days. Therefore, Methadone has worse withdrawal symptoms.
Is it safe to be on MAT long-term?
Yes, medication-assisted treatment (MAT) such as Suboxone and Methadone is considered safe for long-term use, especially when combined with therapy, enhancing recovery outcomes from opioid addiction.
How is Suboxone typically taken?
Suboxone is typically taken daily by placing a sublingual film or tablet under the tongue, allowing it to dissolve and be absorbed effectively. This method ensures optimal delivery of the medication.
Do Methadone clinics provide additional support services?
Methadone clinics do provide additional support services, such as counseling and regular health check-ups, which are essential for effective treatment.