The duration of Suboxone treatment varies widely among individuals. While some may only need it for a few months, others may require it for several years. The key is to follow a treatment plan tailored to your specific needs, as determined by your healthcare provider. In this article, we will explore the factors that influence how long you should be on Suboxone and what to consider as you plan your recovery journey.
Key Takeaways
- Suboxone treatment duration varies for individuals, typically ranging from a few months to several years, based on personal circumstances and medical advice.
- Long-term Suboxone use is often more effective for stable recovery, reducing relapse risks, while short-term treatment may lead to increased chances of relapse.
- Tapering off Suboxone requires a personalized plan supervised by a healthcare provider to ensure safety and effectiveness, with potential for lifelong maintenance in some cases.
What is Suboxone, and how does it work?
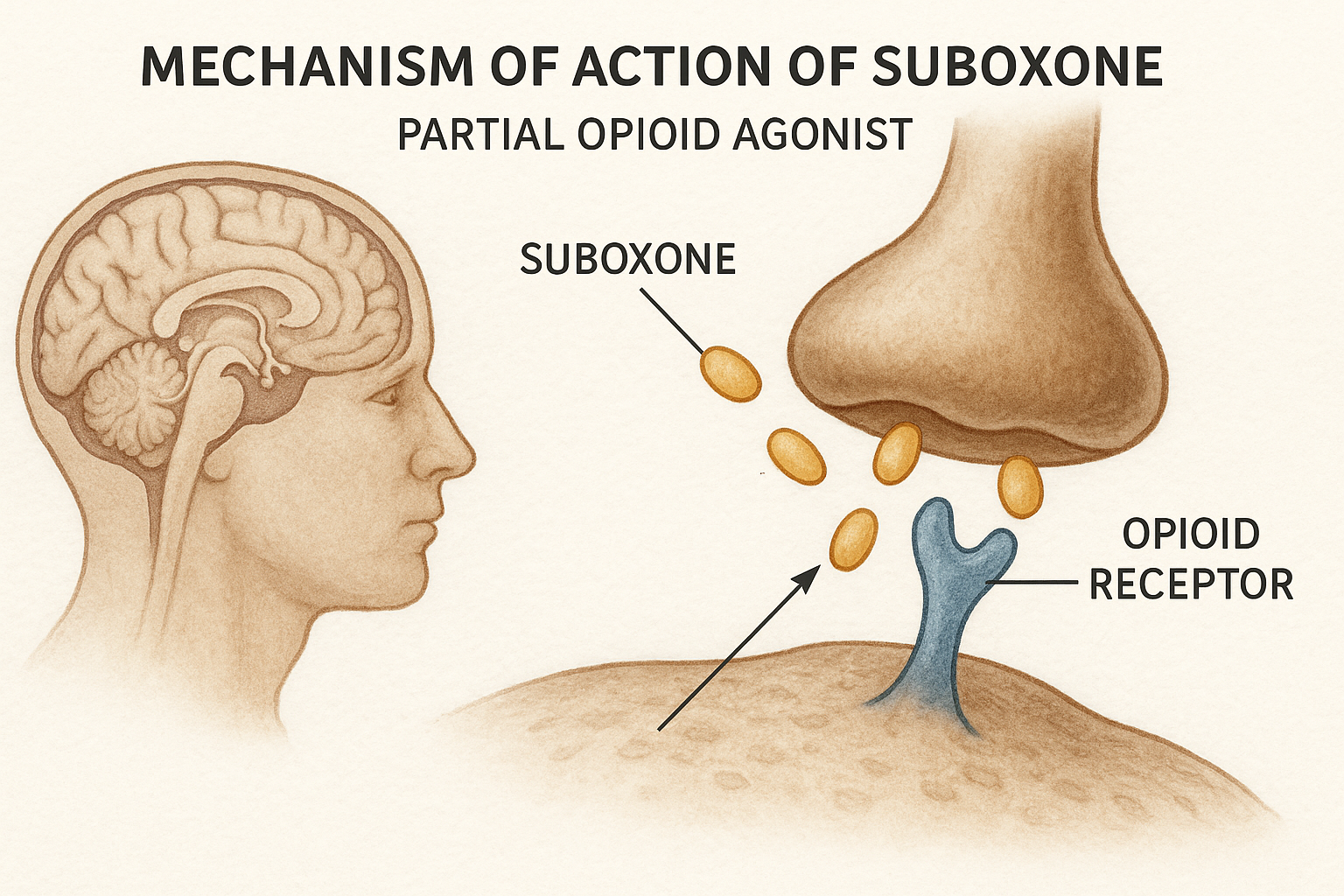
Suboxone is a prescription drug that combines buprenorphine and naloxone to treat opioid addiction. Buprenorphine is a partial opioid agonist, meaning it activates opioid receptors in the brain but to a much lesser extent than full agonists like heroin or oxycodone. This helps reduce cravings and withdrawal symptoms without producing the same intense high.
Naloxone is classified as an opioid antagonist. It works by blocking the effects of opioids. Its primary role in Suboxone is to prevent misuse. If someone tries to inject Suboxone, naloxone will block the opioid effects, causing withdrawal symptoms instead. This combination makes Suboxone a powerful tool in medication-assisted treatment (MAT) for opioid addiction.
To better understand how Suboxone supports recovery, it helps to explore what Suboxone is used for in medication-assisted treatment programs. This action stabilizes brain chemistry, reducing the risk of relapse and allowing individuals to focus on other aspects of recovery, such as therapy and lifestyle changes.
Taking Suboxone as part of a comprehensive treatment plan can significantly improve outcomes in overcoming addiction. Managing drug cravings and withdrawal symptoms with Suboxone helps patients regain control of their lives and work towards long-term recovery. To achieve the best results, it is essential to take suboxone as prescribed.
How long should you be on Suboxone? Short answer explained first
There is no one-size-fits-all timeline for Suboxone treatment. The duration can vary significantly among individuals, ranging from a few months to several years, depending on personal circumstances and medical advice. Patients should always consult their healthcare provider to determine the best approach for their situation.
In general, Suboxone treatment can be categorized into three broad durations:
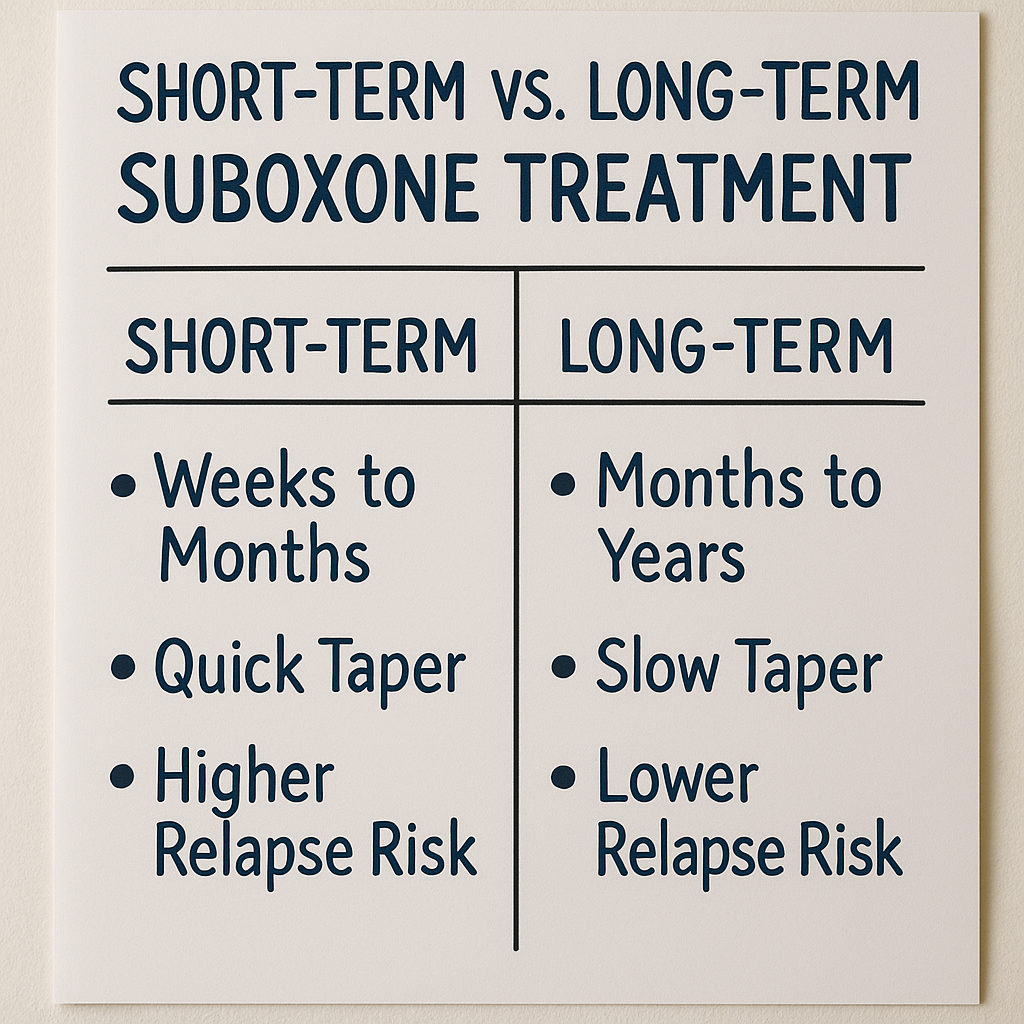
- Short-term treatment: 3–6 months
- Moderate-term: 12–18 months
- Long-term maintenance: 2+ years or indefinite
Long-term use of Suboxone is often recommended, as it can improve recovery stability and reduce the risk of relapse. Short-term treatment of less than a month has been found to be less effective and frequently leads to relapse. The ultimate goal is to help patients achieve a stable recovery while they address other important aspects of their healing journey.
Factors that determine how long you should stay on Suboxone
Several factors influence how long you should stay on Suboxone. One of the most significant is the duration and severity of your opioid addiction. The longer and more severe the addiction, the longer you may need to stay on Suboxone to achieve stable recovery.
Co-occurring mental health conditions, such as depression or anxiety, can also play a role in determining treatment duration. Addressing these conditions alongside opioid addiction can be crucial for a successful recovery. Additionally, your history of cravings and relapse will impact how long you should stay on Suboxone. Those with a strong history of relapse may benefit from longer treatment.
Your support system and recovery environment are also critical factors. A strong support network and a stable environment can significantly enhance recovery outcomes, potentially reducing the time needed on Suboxone.
Lastly, your personal goals and preferences, along with your doctor’s recommendations and the guidelines of your MAT program, will shape your treatment plan. Insurance coverage and access to care can also affect treatment duration. Having the necessary resources and support to stay on Suboxone for as long as needed is vital for a successful recovery.
Short-term vs. long-term Suboxone treatment: Which is better?
Short-term Suboxone treatment typically lasts between three to six months, while long-term treatment can extend to two years or even indefinitely. Each approach has its pros and cons, and comparing Suboxone vs methadone can help determine the most suitable treatment based on individual needs.
Short-term addiction treatment offers the advantage of fewer side effects and a shorter commitment. However, it carries a higher risk of relapse and may not allow enough time for the brain to fully heal from the effects of opioid addiction. Many patients find that short-term treatment alone is insufficient to treat addiction for sustaining long-term recovery.
On the other hand, long-term Suboxone treatment provides:
- Greater stability
- Reduced relapse rates
- More time for patients to build new coping mechanisms
- Opportunity to address underlying issues contributing to their addiction
For those with chronic opioid use disorder, long-term treatment is often more effective in achieving lasting recovery with opioid drugs over an extended period, according to doctors. Other drugs play a significant role in this process.
Studies and expert guidelines from organizations like SAMHSA and NIDA support the benefits of long-term Suboxone use, emphasizing that it offers a higher chance of successful recovery and a lower risk of relapse.
When is the right time to stop taking Suboxone?
Determining the right time to stop taking Suboxone is a highly individualized process. Some signs that you may be ready to taper off include no longer experiencing opioid cravings, having a strong relapse prevention plan in place, and maintaining stable mental health. However, it’s crucial to consult with your healthcare provider before making any changes to your treatment plan.
Stopping Suboxone too early can pose significant risks, including the potential for relapse. It’s essential to have a comprehensive plan and support system to manage any challenges that may arise during the tapering process. Each patient’s journey is unique, and what works for one person may not be suitable for another.
Case-by-case examples highlight the importance of individualized treatment. For instance, someone with a robust support network and minimal relapse history may successfully taper off sooner than someone with multiple relapse episodes and ongoing mental health challenges to prevent relapse.
How to taper off Suboxone safely
Tapering off Suboxone safely requires a well-thought-out plan and close monitoring by a healthcare provider, much like the medical supervision needed during a Suboxone detox, which helps manage withdrawal symptoms and prevent relapse. Unlike quitting cold turkey, which can lead to severe withdrawal symptoms and a high risk of relapse, tapering involves gradually reducing the Suboxone dose over time.
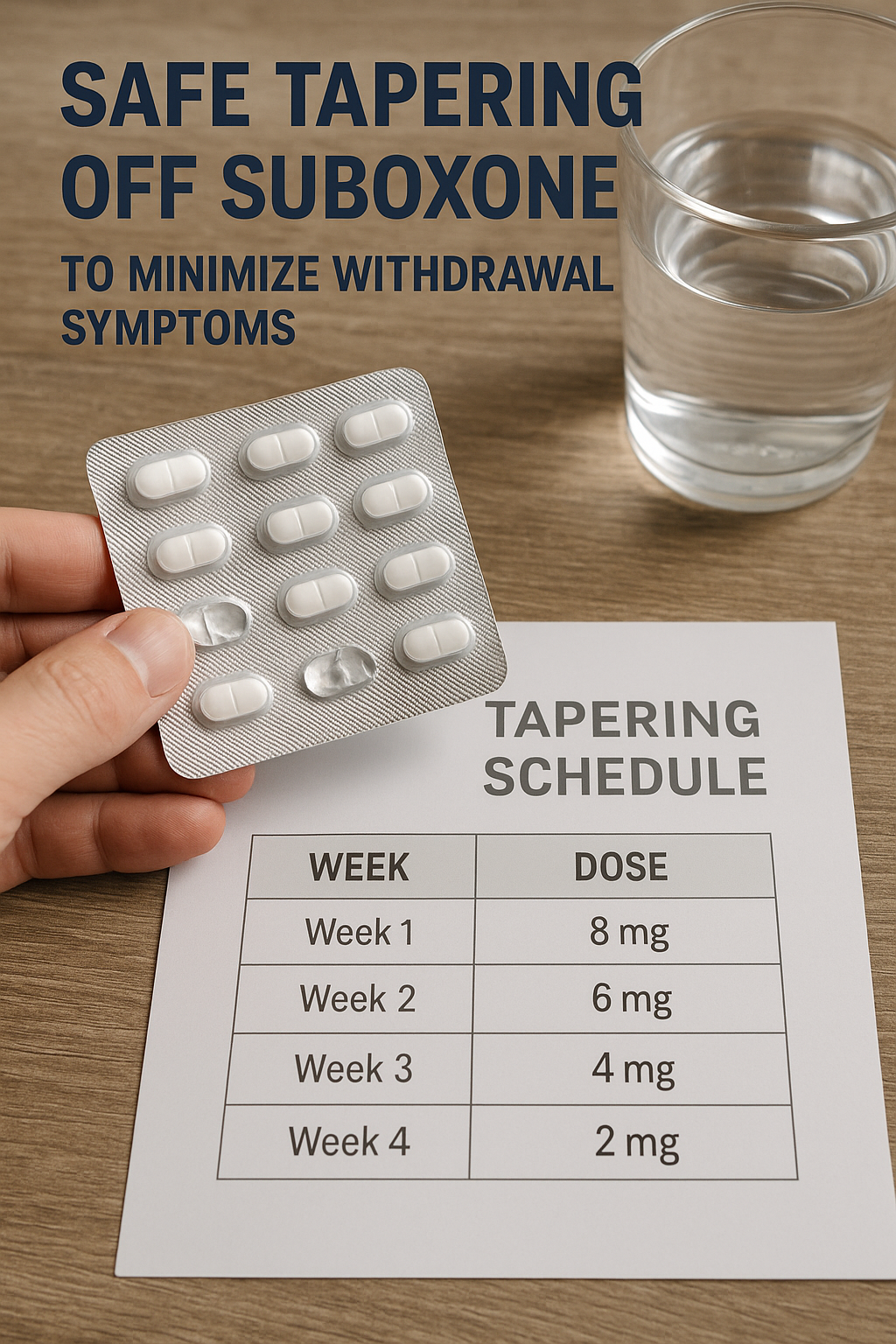
General tapering strategies include gradually decreasing the dose, monitoring withdrawal symptoms, and adjusting the taper pace based on individual responses to reduce withdrawal symptoms. A common tapering schedule might involve reducing the dosage by 2 mg every one to two weeks, but this can vary depending on individual needs and circumstances.
Rapid tapering or self-tapering without medical professional supervision can be dangerous and is not recommended. It’s essential to work closely with your healthcare provider to ensure a safe and effective tapering process.
What happens if you stay on Suboxone long term?
Staying on Suboxone long term is often misunderstood, with some confusing it with Suboxone addiction, even though the medication supports recovery when used as prescribed. However, this is a myth. Evidence-based research supports the safety and effectiveness of long-term Suboxone maintenance in managing opioid addiction.
Common physical effects of long-term Suboxone use can include hormonal changes and dental issues, but these are often manageable with proper medical care. Psychological effects, such as emotional numbing, can also occur, but these are typically outweighed by the benefits of reduced relapse risk and greater stability.
Addiction medicine experts emphasize that long-term use of buprenorphine, the active ingredient in Suboxone, is a legitimate and effective treatment option for many individuals. It provides a stable foundation for recovery, allowing patients to focus on rebuilding their lives without the constant fear of relapse.
Is lifelong Suboxone maintenance ever recommended?
Lifelong Suboxone maintenance may be appropriate for certain individuals, especially those with multiple failed taper attempts, high relapse risk, or chronic opioid dependency. In these cases, the benefits of ongoing Suboxone use far outweigh the potential risks.
Comparisons to other chronic medications, such as insulin for diabetes, highlight the importance of recognizing opioid use disorder as a chronic condition that may require long-term or lifelong management, including the potential for physical dependence. A harm reduction mindset is crucial in addressing opioid addiction, focusing on minimizing negative outcomes and improving overall quality of life, as some strategies may be misused.
Lifelong maintenance treatment is not a failure but a valid treatment option for those who need it. It ensures that patients can lead healthier, more stable lives while managing their addiction effectively.
Patient experiences: Real stories and outcomes
Hearing from those who have walked the path of Suboxone treatment can provide valuable insights and inspiration. For example, some patients have successfully tapered off Suboxone after short-term use, while others have found long-term maintenance to be the key to their recovery.
Testimonials from those who have tapered off successfully often highlight the importance of a strong support system and a gradual tapering plan. Different paths and definitions of success show that recovery is a deeply personal journey, and there is no one-size-fits-all solution.
These real-life stories underscore the importance of individualized treatment plans and the vital role of Suboxone in helping patients reclaim their lives from opioid addiction.
Bottom line: How long should you be on Suboxone?
The duration of Suboxone treatment is highly individual and should be tailored to each patient’s needs. It’s essential to work closely with your healthcare provider to create a personalized treatment timeline that supports your recovery goals.
Medical supervision and evidence-based care are crucial in determining the right duration for Suboxone use. Don’t rush off medication if it supports your recovery. Speak with your provider or addiction specialist to ensure you make the best decision for your long-term health.
FAQs About Suboxone Duration
Can you be on Suboxone for life?
Yes, lifelong Suboxone maintenance can be recommended for those with chronic opioid use disorder, especially if they have a high risk of relapse or have not succeeded in tapering off before.
Is 2 years too long to be on Suboxone?
Two years on Suboxone is not considered too long; it can be a beneficial duration for many patients in their recovery process.
Can you relapse if you stop Suboxone after 6 months?
Stopping Suboxone after 6 months can indeed lead to a risk of relapse, particularly if adequate relapse prevention strategies are not in place. It is crucial to have a solid plan and support system when considering discontinuation.
How does Suboxone affect the brain long term?
Long-term use of Suboxone stabilizes brain chemistry and lowers relapse risk, but it requires consistent monitoring by a healthcare provider to ensure safety and effectiveness.
What are the side effects of long-term Suboxone use?
Long-term use of Suboxone can lead to hormonal changes and dental issues, which can be effectively managed with proper care. It’s important to monitor these side effects for ongoing well-being.