Switching from methadone to Suboxone involves important steps to ensure it’s done safely under medical supervision. This guide will explain how to taper methadone, the waiting period needed, and how to start Suboxone to avoid withdrawal symptoms. You’ll also learn why this switch might be beneficial and what to expect during the process.
Key Takeaways
- Transitioning from methadone to Suboxone must occur under medical supervision to mitigate the risk of precipitated withdrawal, emphasizing the importance of timing and tapering.
- Candidates for the switch typically include individuals on lower methadone doses and those with strong support systems, who are prepared for the change and have a stable recovery environment.
- Suboxone offers greater treatment flexibility and a reduced risk of misuse compared to methadone, making it an appealing option for many patients seeking long-term recovery.
Can you switch from methadone to Suboxone safely?
Switching from methadone to Suboxone can be done safely under the right conditions. This transition requires a careful reduction of methadone under medical supervision to avoid precipitated withdrawal. Precipitated withdrawals can occur if Suboxone is introduced too soon after methadone, due to the differences in how these medications interact with opioid receptors.
Gradually reducing the methadone dose under medical supervision ensures a smooth and safe transition. This process minimizes withdrawal symptoms and prepares the body for Suboxone. The switch should be tailored to individual health needs, considering factors such as current methadone dose, overall health, and treatment goals.
The decision to switch should be made with a healthcare provider who can assess readiness and develop a personalized transition plan. Patients who are stable on methadone and have strong support systems are often good candidates for this switch.

What makes the switch medically sensitive?
The transition from methadone to Suboxone is medically sensitive primarily due to the risk of precipitated withdrawal. Precipitated withdrawal occurs when:
- Buprenorphine, a partial opioid agonist in Suboxone, displaces methadone, a full opioid agonist, from opioid receptors too quickly.
- This rapid displacement can lead to severe withdrawal symptoms, including nausea, vomiting, sweating, and anxiety.
- Because of these risks, the timing of the switch is critical.
Buprenorphine binds to opioid receptors without producing the same euphoria as methadone. Important considerations include:
- If introduced too soon, buprenorphine can displace methadone, causing intense withdrawal.
- Patients need to experience mild to moderate withdrawal symptoms before initiating Suboxone.
- This ensures buprenorphine binds effectively without causing severe discomfort.
Additionally, comorbid medical or psychiatric conditions can complicate the transition. Patients with heart problems, liver issues, or other significant health concerns need careful evaluation and possibly a modified transition plan for transferring patients to ensure their safety during the switch. These conditions highlight the need for personalized medical supervision during the transition.
Who is a good candidate for switching?
Candidates usually include those on lower methadone doses (under 30-50 mg/day) and with a stable recovery environment. Employment, strong support systems, and stable housing significantly contribute to a successful transition for stable methadone maintenance patients and methadone maintained subjects. Individuals who meet these criteria are generally better positioned to manage the challenges of switching medications through methadone maintenance treatment, higher methadone doses, methadone maintenance therapy, and methadone maintenance.
Health considerations are also important. Patients with a history of managing withdrawal or medication changes may need closer evaluation. Existing medical issues, such as heart problems or liver conditions, must be taken into account to determine whether Suboxone is a safer option.
Personal goals and readiness for change are equally important, as a motivated and well-prepared individual is more likely to benefit from the switch.
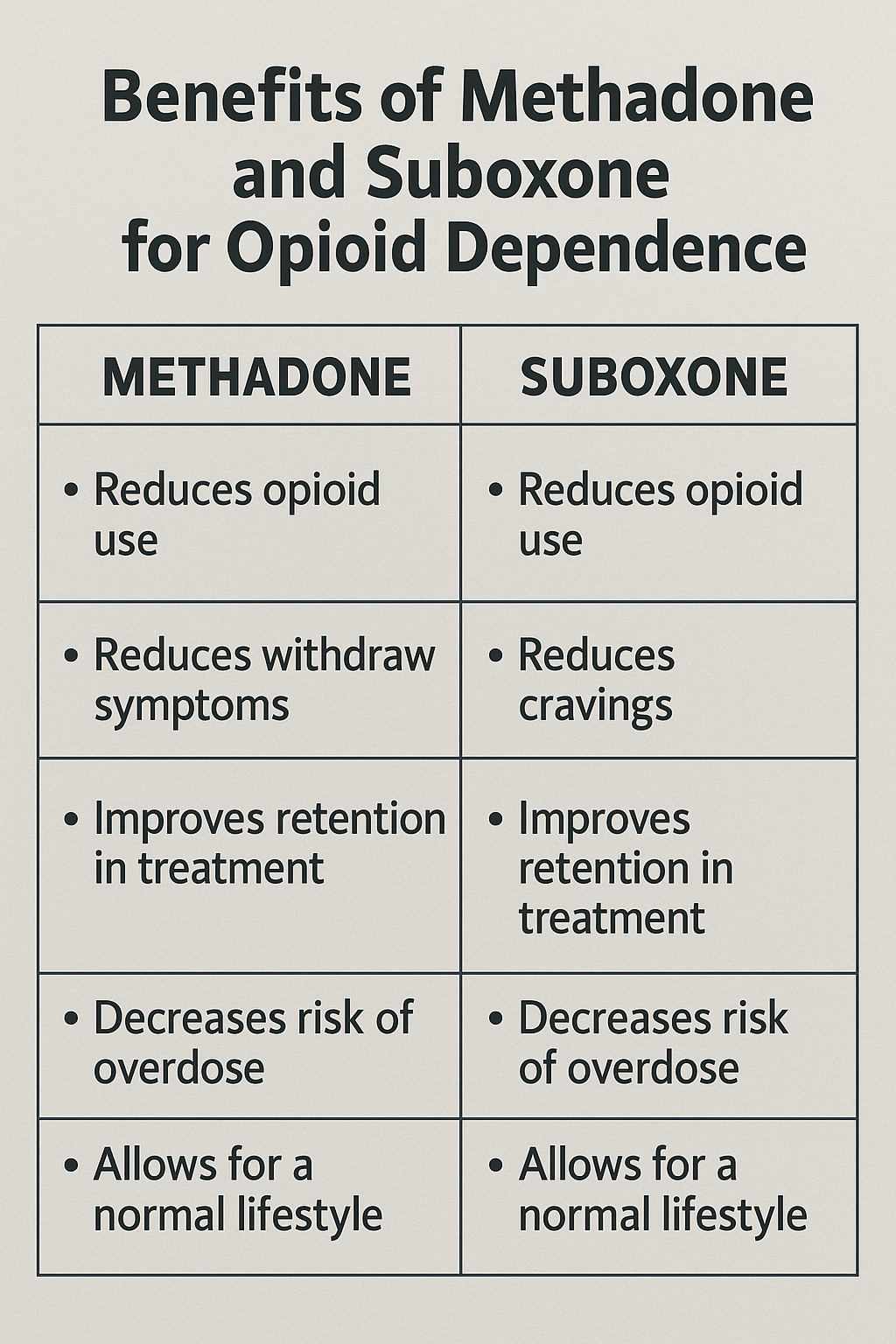
Methadone vs. Suboxone: Which is better for long-term recovery?
Both methadone and Suboxone are effective in reducing opioid cravings and improving long-term treatment outcomes for individuals with opioid use disorder. However, each medication has distinct advantages suited to different levels of opioid dependence. Methadone is often preferred for individuals with severe dependence due to its full agonist properties, which provide significant stabilization. Suboxone, on the other hand, is beneficial for those seeking a treatment option with a lower risk of misuse and overdose.
Choosing between methadone and Suboxone depends on factors like dependence severity, treatment goals, and the need for treatment flexibility:
- Methadone is effective for high-dependency individuals.
- Suboxone offers more outpatient flexibility.
- Suboxone has a safer profile for moderate dependence.
Methadone excels at high-dependency stabilization; Suboxone reduces misuse risks
Methadone effectively stabilizes individuals with high levels of opioid addiction. Its full opioid agonists properties mean it occupies opioid receptors completely, reducing cravings and withdrawal symptoms significantly. This makes methadone an ideal option for those with severe opioid use disorder, as it helps maintain opioid tolerance at higher doses and supports long-term stabilization, particularly through the mu opioid receptor. Opioid agonists like methadone play a crucial role in this process.
Suboxone, on the other hand, includes naloxone, which helps prevent misuse by inducing withdrawal symptoms if misused. Buprenorphine in Suboxone provides relief from withdrawal symptoms while minimizing overdose risk. This combination makes Suboxone a safer option for those concerned about the potential for misuse and seeking a treatment that reduces the risk of dependency.
Suboxone offers outpatient flexibility and lower overdose risk
Suboxone’s safety features include:
- Its partial agonist nature creates a ceiling effect, significantly lowering the likelihood of overdose compared to full agonists like methadone.
- The ceiling effect ensures that beyond a certain dose, Suboxone does not produce additional opioid effects, reducing the risk of respiratory depression and overdose.
- The presence of naloxone acts as a deterrent against injection misuse, further enhancing its safety profile.
Suboxone can be prescribed for at-home use, allowing patients to manage their treatment without the need for daily visits to a methadone clinic in an outpatient setting. This flexibility supports long-term recovery by allowing patients to integrate treatment into their daily lives, maintaining work and family responsibilities.
The convenience and autonomy of Suboxone make it attractive for those seeking flexible treatment.
How to transition from methadone to Suboxone: Step-by-step process
Transitioning from methadone to Suboxone requires a structured and monitored process to ensure safety and minimize withdrawal symptoms. This process includes tapering the methadone dose, waiting after the last dose, and starting Suboxone induction under medical supervision. Each of these steps plays a crucial role in ensuring a smooth and successful transition.
Following a structured approach is crucial to avoid complications like precipitated withdrawal and ensure a comfortable transition.
Healthcare providers guide patients through the process, offering support and making adjustments based on the patient’s response.
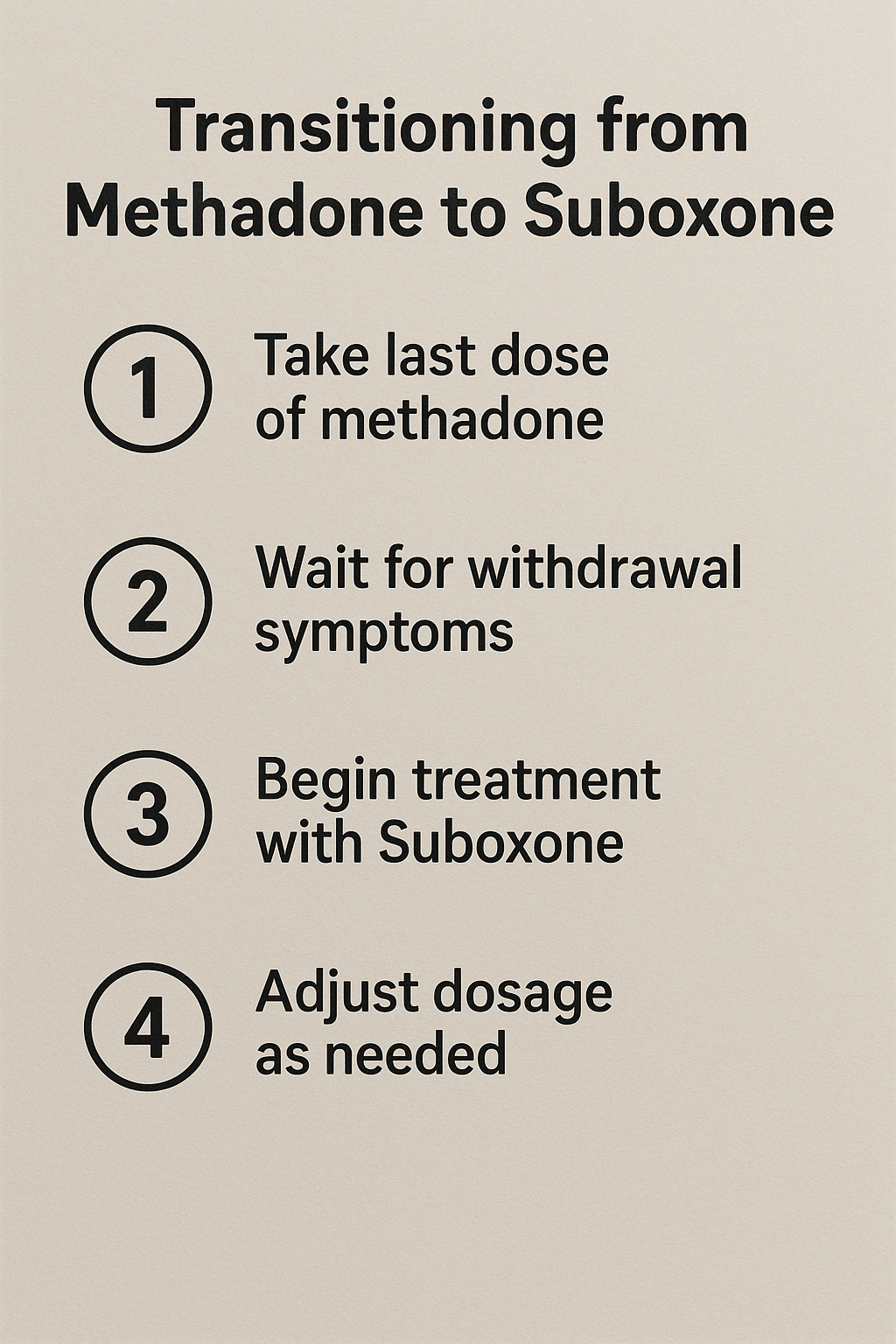
Step 1: Taper methadone to ≤30 mg/day
The first step is to gradually reduce the methadone dose to 30 mg per day or less. This process:
- Reduces the risk of severe withdrawal symptoms when switching to Suboxone.
- Requires patients to work closely with their healthcare provider to determine an appropriate tapering schedule.
- Aims to minimize discomfort while preparing the body for the switch.
A gradual reduction allows the body to adjust, making the transition smoother and less disruptive. Following the tapering plan carefully and not rushing the process helps avoid increased withdrawal symptoms and complications.
Step 2: Wait 24–72 hours after last dose
After reaching 30 mg per day or less, patients should wait 24 to 72 hours after their last methadone dose before starting Suboxone. This waiting period is essential to allow mild to moderate withdrawal symptoms to develop, which indicates that the methadone has sufficiently cleared from the body.
The Clinical Opiate Withdrawal Scale (COWS) can help determine the right timing, with a score of 13 or higher indicating readiness. This waiting period helps to prevent precipitated withdrawal, which can occur if Suboxone is started too soon.
Patients should be closely monitored to manage withdrawal symptoms and ensure readiness for the next step.
Step 3: Begin Suboxone induction with a medical provider
The final step is to start buprenorphine induction under medical supervision. This typically involves:
- Starting with a low dose of Suboxone, such as 2-4 mg of buprenorphine
- Monitoring the patient’s response
- Carefully adjusting the initial dose based on the patient’s withdrawal symptoms and overall response to the medication.
Continuous follow-up during the induction phase ensures:
- The patient receives the right first dose
- Management of any side effects or withdrawal symptoms
- Monitoring that balances symptom relief with side effect avoidance
- A smooth transition
What are the risks and side effects of switching?
Switching from methadone to Suboxone involves potential risks and side effects, mainly related to withdrawal symptoms and timing. If not managed properly, the transition can lead to severe withdrawal symptoms, including:
- anxiety
- nausea
- vomiting
- sweating
- irritability
These symptoms can be distressing and may increase the risk of relapse if not adequately addressed.
Proper timing and medical supervision minimize these risks. Patients must follow the recommended tapering schedule and waiting period to reduce severe withdrawal symptoms. Monitoring and support from healthcare providers are essential for managing these risks and ensuring a successful transition.
Common risks: withdrawal symptoms and poor timing
A significant risk during the transition is precipitated withdrawal, which can occur if Suboxone is started too soon after the last methadone dose. This happens because buprenorphine in Suboxone displaces methadone from opioid receptors, leading to rapid onset of withdrawal symptoms. Proper timing is critical to avoid this complication, with a recommended waiting period of 24 to 72 hours after the last methadone dose.
Patients should be closely monitored during the waiting period to ensure withdrawal symptoms are at the appropriate level before starting Suboxone. Starting Suboxone too early can worsen withdrawal symptoms, making the transition difficult and uncomfortable.
Side effects to expect during transition
During the transition, patients may experience side effects like:
- nausea
- headaches
- irritability
- insomnia
These symptoms are typically related to opioid or Suboxone withdrawal and can vary in intensity depending on the individual and the specifics of the tapering and induction process, including mild withdrawal symptoms, illicit opioids, and opioid addiction.
In addition to these common withdrawal symptoms, patients may also experience gastrointestinal issues and respiratory depression, which require careful monitoring and management. The duration of these symptoms varies, but they usually subside as the body adjusts to Suboxone. It is important for patients to communicate with their healthcare provider about any side effects they experience to receive appropriate support and treatment.
Why do people switch from methadone to Suboxone?
Many switch from methadone to Suboxone due to the lower risk of overdose from buprenorphine’s ceiling effect and increased treatment flexibility. Suboxone allows patients to take medication at home, eliminating the need for daily clinic visits. This flexibility can significantly enhance the quality of life for those with daily responsibilities.
Additionally, Suboxone is often perceived as less stigmatizing compared to methadone treatment. Patients often feel less judged and more integrated into their communities when using Suboxone. The ability to manage treatment privately can help individuals maintain their dignity and reduce the negative social implications associated with methadone clinics.
Increased independence and outpatient convenience
Suboxone’s take-home format offers several advantages:
- Allows patients to maintain their treatment without constant supervision, providing greater autonomy and independence.
- Unlike methadone, which requires daily clinic visits, Suboxone can be prescribed for at-home use, reducing the need for regular visits.
- This flexibility allows individuals to integrate their treatment into their daily lives more seamlessly.
The ability to manage Suboxone treatment at home can significantly enhance the quality of life for individuals balancing work or education commitments. This flexibility and convenience are major motivators for individuals considering the switch from methadone to Suboxone.
Lower stigma and better life integration
Switching to Suboxone may reduce the stigma of opioid treatment, as patients can avoid the visible identification often associated with methadone clinics. Many patients report feeling more empowered and able to integrate their recovery into daily life after switching to Suboxone due to its flexibility. This can lead to a greater sense of normalcy and improved social interactions.
The private nature of Suboxone treatment can enhance patients’ dignity, allowing for a more integrated lifestyle while in recovery. Reducing healthcare visits contributes to a more routine lifestyle, allowing individuals to maintain employment and family responsibilities without frequent clinic disruptions.
What doctors and studies say about switching
Medical professionals and studies offer valuable insights into switching from methadone to Suboxone. Clinical guidelines emphasize reducing methadone doses before transitioning to buprenorphine substitution therapy to minimize withdrawal risks. These guidelines are supported by extensive research and recommendations from leading organizations such as the Substance Abuse and Mental Health Services Administration (SAMHSA) and the American Society of Addiction Medicine (ASAM).
Insights from clinical studies highlight success rates and strategies for minimizing withdrawal symptoms during the transition. These studies provide critical information on the effectiveness of different tapering protocols and the need for individualized treatment plans to ensure a safe and successful switch.
SAMHSA and ASAM guidelines
SAMHSA and ASAM guidelines recommend initiating buprenorphine treatment only when patients exhibit moderate opioid withdrawal symptoms. This allows buprenorphine to bind effectively to opioid receptors. As a result, it does not lead to precipitated withdrawal. SAMHSA emphasizes the importance of proper timing and dosage adjustments for a smooth transition.
ASAM guidelines advocate for psychosocially assisted pharmacological treatment, including comprehensive support for the psychological and social aspects of addiction. These guidelines highlight the need for a holistic approach, combining medication assisted treatment with substance abuse treatment and support services to improve outcomes.
Clinical study findings on taper and transition outcomes
Clinical studies show that transitioning from methadone to buprenorphine doses can be successfully managed, particularly when a lower pretransfer methadone dose is established before high dose methadone transfer occurs after methadone doses are reduced to 30-50 mg/day before the switch. In one study, approximately 79% of participants remained on buprenorphine treatment one week after transferring from methadone, indicating a high success rate. These findings underscore the importance of careful daily methadone dose management and monitoring during the transition.
Research highlights the need for individualized treatment plans to address each patient’s unique needs. Strategies such as gradual tapering and close monitoring can help minimize withdrawal symptoms and improve the overall success of the transition.
Participants reported improved quality of life scores after switching to buprenorphine, indicating positive health outcomes from the transition.
Tips for a smoother transition
To ensure a smoother transition, maintaining open communication with healthcare providers is crucial. Patients should work with their healthcare provider to create a tailored transition plan addressing their specific needs and concerns. The plan should include a gradual tapering schedule, proper timing, and continuous monitoring to manage withdrawal symptoms effectively.
It is also important for patients to be patient and not rush the withdrawal period. Gradually tapering off methadone reduces the severity of withdrawal symptoms and prepares the body for Suboxone. Following the recommended waiting period and starting Suboxone under medical supervision enhances the transition’s success.
Work with a Suboxone-certified provider
Working with online Suboxone doctors enhances the chances of a safe and effective transition by offering remote access to experienced care. These providers:
- Have specialized training and experience in managing the complexities of transitioning from methadone to Suboxone
- Offer personalized guidance and support tailored to the patient’s needs
- Ensure a smoother and more successful switch
A certified Suboxone provider prescribes the medication, monitors progress, and adjusts treatment plans as needed. This ongoing support is essential for managing withdrawal symptoms and addressing any challenges that may arise during the transition.
Finding a provider with experience in transitioning patients from methadone can make a significant difference in the overall success of the process.
Don’t rush the withdrawal period
Patience is key when transitioning from methadone to Suboxone. Gradually tapering off methadone helps reduce the severity of withdrawal symptoms and allows the body to adjust to lower opioid levels. Rushing the withdrawal period can lead to increased discomfort and complications, making the transition more challenging.
Following the recommended waiting period and starting Suboxone under medical supervision is critical to ensuring a smooth transition. This approach helps minimize withdrawal symptoms and supports a more comfortable and successful switch.
Patients should communicate regularly with their healthcare provider and follow their guidance closely to achieve the best possible outcomes.
Bottom Line: Making the switch safely and successfully
Creating a safe and effective transition from methadone to Suboxone requires careful medical oversight and patient support. It is essential to follow the recommended steps:
- Taper methadone doses gradually.
- Wait the appropriate period before starting Suboxone.
- Start Suboxone under medical supervision.
- Use adjunctive medications to help alleviate withdrawal symptoms during the transition process.
Individual patient history and comorbidities should guide the transition plan to minimize risks and ensure the best possible outcomes. With the right support and a well-structured plan, patients can successfully make the switch from methadone to Suboxone, improving their chances of long-term recovery and a better quality of life.
FAQs about switching from methadone to Suboxone
How long does it take to switch from methadone to Suboxone?
Switching from methadone to Suboxone typically takes 1 to 3 weeks, involving a gradual tapering of methadone and a waiting period of 24 to 72 hours after the last methadone dose before initiating Suboxone.
Can you switch from high-dose methadone to Suboxone?
Switching from high-dose methadone to Suboxone is not advisable without a proper tapering period, as it can lead to precipitated withdrawal. A gradual taper is essential to reduce withdrawal symptoms effectively.
Is switching better than staying on methadone?
Switching from methadone to Suboxone may be beneficial for some individuals seeking increased flexibility and reduced stigma, but the effectiveness of methadone for severe opioid dependence should not be overlooked. Ultimately, the decision should align with personal treatment goals and stability.
What are the risks of switching too quickly?
Switching too quickly poses significant risks, such as severe withdrawal symptoms like anxiety, nausea, and vomiting. Therefore, it is essential to ensure proper timing and seek medical supervision during this process.
Why do people switch from methadone to Suboxone?
People often switch from methadone to Suboxone due to its lower risk of overdose and greater treatment flexibility, which facilitate better integration into daily life. This transition can also help reduce the stigma associated with opioid addiction.
















