If you’re considering naltrexone for opioid or alcohol dependence, understanding its side effects of naltrexone is crucial. From common issues like nausea and fatigue to more serious concerns such as liver toxicity and allergic reactions, being informed helps you manage risks better.
Key Takeaways
- Naltrexone can cause both physical and psychological side effects, with common issues including nausea, fatigue, anxiety, and sleep disturbances, particularly during the initial stages of treatment.
- It is crucial to monitor liver function and be aware of severe side effects like liver toxicity and allergic reactions, as these can require immediate medical attention.
- Gender differences impact naltrexone efficacy and side effects, with women experiencing higher rates of nausea and poorer treatment outcomes, emphasizing the need for personalized approaches in therapy.
What are the most common side effects of naltrexone?
Naltrexone, a medication primarily used to treat opioid and alcohol addiction, is known for a range of side effects. The most frequently reported include gastrointestinal issues like nausea and vomiting, as well as fatigue and insomnia. These side effects can vary in intensity and duration, and understanding them is crucial for those starting naltrexone therapy.
The following sections will delve into the short-term physical and psychological side effects one might experience during the early stages of naltrexone treatment.

Short-term physical side effects
Short-term physical side effects of taking naltrexone often emerge within the first few days or weeks of treatment. These commonly include:
- Nausea
- Stomach cramps
- Joint and muscle pain
- Headaches
While these symptoms can be uncomfortable, they are usually temporary and tend to subside as the body adjusts to the medication.
Patients should report any persistent or severe symptoms to their healthcare provider and tell your doctor for proper management and support.
Short-term psychological side effects
In addition to physical symptoms, some individuals may experience psychological side effects shortly after starting naltrexone. These can include increased anxiety, mood swings, and sleep disturbances such as trouble sleeping or insomnia. Anxiety levels may spike particularly during the initial month of treatment.
While some patients might experience a reduction in depressive symptoms over time, it’s essential to monitor these psychological effects closely and seek support from mental health services administration if needed.
How serious are naltrexone’s side effects?
The severity of naltrexone’s side effects can range from mild to severe. Mild side effects might include minor gastrointestinal discomfort or fatigue, which generally do not require medical intervention. Moderate side effects may be more bothersome and could necessitate dosage adjustments or additional treatment.
Severe side effects, though rare, require immediate medical attention. These can include significant liver dysfunction, allergic reactions, or severe psychological symptoms. Being able to identify these side effects and knowing when to seek help is crucial for anyone on naltrexone therapy.

Liver toxicity and elevated liver enzymes
Naltrexone can affect liver function, particularly at higher doses. While the FDA removed the black-box warning regarding liver toxicity in 2013 due to the absence of reported hepatic failure cases, it is still important to monitor liver enzyme levels regularly. Elevated liver enzymes are mostly mild and self-limiting but can indicate liver damage.
Symptoms of liver toxicity include jaundice, fatigue, and abdominal pain. Regular liver function tests are recommended to ensure any potential issues are caught early.
Allergic reactions and anaphylaxis
Although rare, naltrexone can cause serious allergic reactions such as rash, swelling, or difficulty breathing. Anaphylaxis, a severe allergic reaction, requires immediate medical attention. Symptoms may include a skin rash, trouble breathing, and swelling of the face or throat.
Patients should be aware of these symptoms and seek medical help promptly if they experience any signs of a serious allergic reaction or an allergic reaction.
Precipitated withdrawal in opioid users
Starting naltrexone too soon after opioid use can trigger precipitated withdrawals, a sudden onset of withdrawal symptoms. This occurs because naltrexone blocks opioid receptors, preventing opioids from exerting their effects and abruptly causing withdrawal symptoms.
To prevent this, individuals must ensure that opioid medications are fully cleared from their system before beginning naltrexone treatment. This highlights the importance of a medically supervised withdrawal process.
Does naltrexone affect men and women differently?
Research indicates that naltrexone may affect men and women differently:
- Men have shown significant reductions in cocaine and alcohol use when they treat alcohol with naltrexone.
- Women tend to have poorer outcomes with naltrexone treatment.
- Women are more likely to discontinue treatment due to severe pre-treatment psychiatric issues.
- Women may also discontinue treatment because of nausea during treatment.
Additionally, higher rates of nausea have been reported in women, which can affect their adherence to the treatment regimen. These gender-related differences underscore the need for tailored approaches in naltrexone therapy.
Side effects by form: oral tablet vs. Vivitrol injection
Naltrexone hydrochloride is available in two forms: oral tablets (Revia) and extended-release injectable (Vivitrol). Each form has its own set of side effects and considerations. Understanding these differences can help patients and healthcare providers choose the most suitable form of naltrexone for individual needs.
The following sections will explore the specific side effects associated with oral and injectable naltrexone.
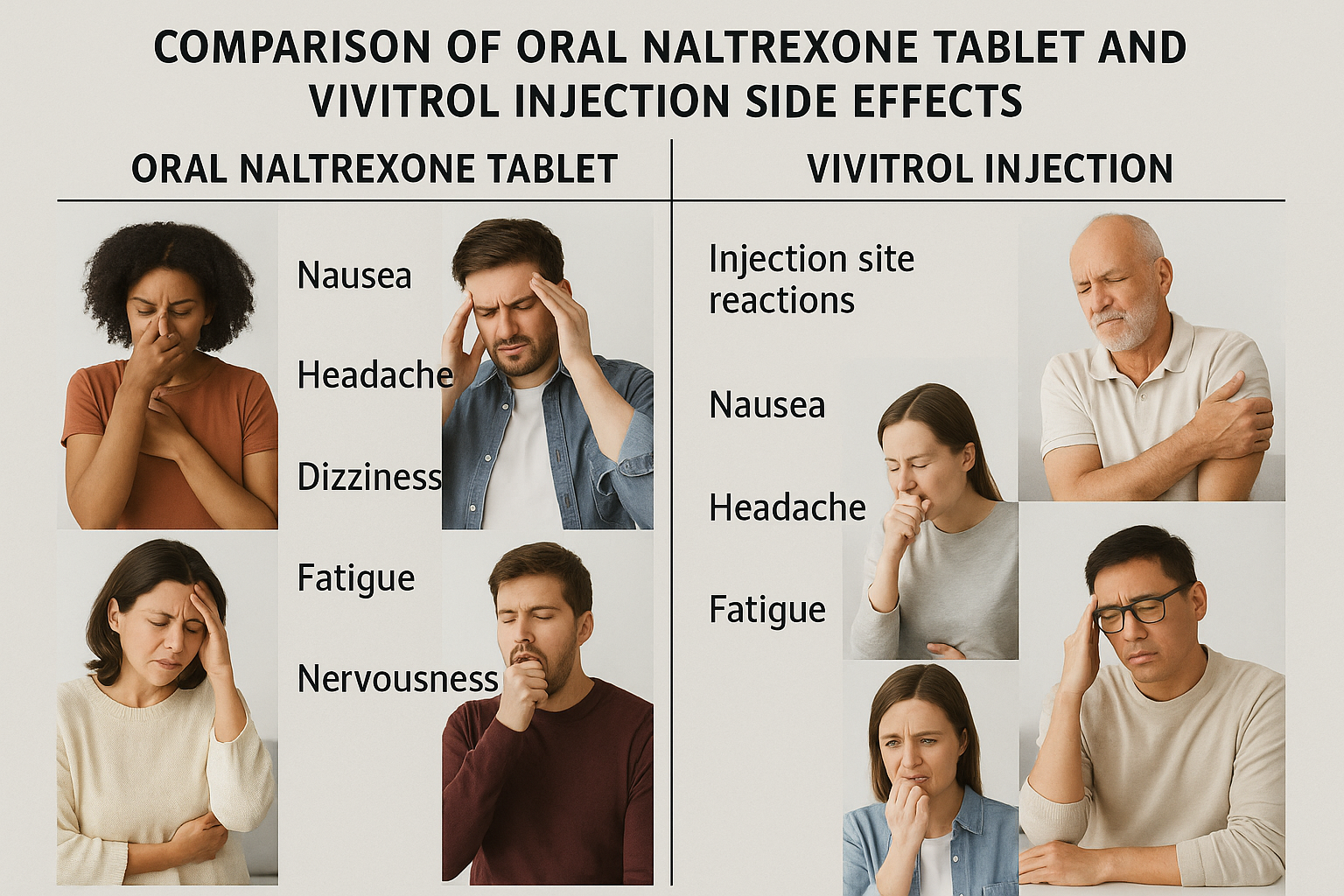
Oral naltrexone (Revia) side effects
Common side effects of oral naltrexone include:
- Gastrointestinal issues such as nausea, vomiting, and stomach cramps
- Headaches
- Dizziness
- Fatigue
- Psychological effects like anxiety and difficulty sleeping
While these side effects can be challenging, they often diminish as the body acclimates to the medication.
Injectable naltrexone (Vivitrol) side effects
Injectable naltrexone (Vivitrol) can cause reactions at the injection site, including soreness, swelling, and redness. Some individuals may experience nausea after the first intramuscular injection, which typically improves with subsequent doses. Serious allergic reactions and symptoms of liver dysfunction, such as dark urine and jaundice, are also possible.
Patients should be aware of these potential side effects and consult their healthcare provider if they experience any following symptoms.
Who is most at risk of naltrexone side effects?
Certain individuals are more at risk of experiencing side effects from naltrexone. These include:
- People with pre-existing liver conditions
- People with kidney impairment
- People with recent opioid use
- People with mental health disorders
Understanding these risk factors can help patients and healthcare providers take necessary precautions to minimize side effects.
The subsections below will delve into the specific risks for people with liver disease and those using opioids before detoxification.
People with pre-existing liver disease
Individuals with liver disease, such as cirrhosis or hepatitis, are at a heightened risk of liver damage when taking naltrexone. Patients should inform their healthcare provider about any liver conditions before starting treatment. Monitoring liver function through regular tests is essential to detect any potential issues early.
Symptoms indicating a serious liver problem, like fatigue, unusual tiredness, unusual bruising, and jaundice, should prompt immediate medical consultation.
People using opioids before detoxification
For individuals who have not fully detoxed from opioids, starting naltrexone can trigger precipitated opioid withdrawal. This is because naltrexone blocks opioid receptors, abruptly cutting off the effects of opioids and causing opioid withdrawal symptoms.
It is vital for these patients to undergo a medically supervised withdrawal process to ensure all opioids are cleared from their system before starting naltrexone.
Can naltrexone side effects be managed or prevented?
Managing or preventing side effects of naltrexone often involves a combination of medical monitoring and lifestyle adjustments. Regular medical assessments and adjusting dosages as needed are key strategies. Additionally, adopting a healthy lifestyle can significantly reduce discomfort when you take naltrexone.
The subsections below will explore specific strategies for medical treatment monitoring and lifestyle adjustments.
Medical monitoring and liver enzyme tests
Regular liver function tests are recommended for individuals on naltrexone to monitor enzyme levels and detect potential liver issues early. These tests should be conducted before, during, and after treatment to track any changes in enzyme levels.
While serious injury liver damage is rare, monitoring is crucial to ensure the safety and effectiveness of the treatment.
Lifestyle adjustments
Incorporating a healthy diet and regular exercise can help mitigate some side effects associated with naltrexone. Staying hydrated is also important, as it can help manage certain side effects like headaches and digestive discomfort. Practicing stress-reduction techniques, such as mindfulness or yoga, can improve psychological well-being during treatment.
Establishing a regular sleep schedule may help reduce sleep disturbances.
How long do naltrexone side effects last?
The majority of naltrexone side effects typically resolve within a few days to weeks as the body adjusts to the medication. If side effects persist beyond this period or become bothersome, it is advisable to consult a healthcare professional.
Most side effects are temporary, but persistent issues should be addressed promptly to ensure the treatment’s effectiveness and the patient’s well-being.
When should you stop taking naltrexone due to side effects?
Patients should discontinue naltrexone if they experience severe side effects such as liver dysfunction, allergic reactions, or significant psychological symptoms. Immediate cessation is also advised if symptoms of precipitated withdrawal occur after taking the medication while opioids are still in the system.
Consulting a healthcare provider is crucial if side effects interfere with daily life or if there are concerns about discontinuing treatment.
Is naltrexone safer than other MAT options?
Naltrexone is considered a non-addictive medication that helps reduce opioid cravings and the risk of relapse. When comparing its safety profile with other MAT options like Suboxone and methadone, naltrexone’s non-addictive nature is a significant advantage. Additionally, non opioid medications can also play a role in managing pain without the risks associated with opioids.
The subsections below will compare naltrexone vs suboxone and methadone in terms of side effects and safety.
Naltrexone vs. Suboxone
Naltrexone and Suboxone (buprenorphine-naloxone) serve different roles in addiction treatment. Naltrexone is an opioid antagonist that blocks opioid effects and reduces cravings without causing dependence. In contrast, Suboxone is a partial agonist that helps manage withdrawal symptoms but carries a risk of dependency.
While naltrexone has a minimal risk of addiction, it requires patients to be opioid-free for 7-14 days before starting to avoid precipitated withdrawal. Suboxone, on the other hand, can be started while patients are still experiencing mild withdrawal symptoms.
However, Suboxone’s opioid nature means it can cause sedation and has a potential for misuse. Therefore, naltrexone may be considered safer for long-term use, especially for those concerned about the risk of developing a new dependency.
Naltrexone vs. Methadone
Methadone, unlike naltrexone, is a full opioid agonist that reduces withdrawal symptoms and cravings by slowly activating opioid receptors. This can help stabilize patients but also carries a risk of physical dependence and potential misuse of opioid medicine, opioid drugs, and other opioids.
Naltrexone, being an opioid antagonist, prevents opioids from producing euphoric effects and does not cause dependency. Starting naltrexone requires a detox period of 7 to 10 days opioid-free, which can be challenging.
Learn more about their key differences in our guide on suboxone vs methadone. Methadone and naltrexone differ in the following ways:
- Methadone is often dispensed through specialized clinics.
- Naltrexone can be prescribed by any healthcare provider, making it more accessible.
- Long-term, naltrexone might be preferred for its non-addictive properties.
- Naltrexone is easier to discontinue without withdrawal symptoms.
Bottom Line: Side Effects of Naltrexone
Understanding the side effects of naltrexone is crucial for anyone considering or currently undergoing treatment. While common side effects like nausea, fatigue, and headaches typically resolve within a few weeks, more serious effects such as liver toxicity or allergic reactions require immediate medical attention. Gender differences in response to naltrexone highlight the need for tailored treatment approaches. Comparing the side effect profiles of naltrexone with other MAT options like Suboxone and methadone underscores its advantages, particularly its non-addictive nature. Through regular medical monitoring and lifestyle adjustments, many side effects can be managed effectively, ensuring a safer and more comfortable treatment experience. Ultimately, informed decision-making and close communication with healthcare providers are key to navigating naltrexone therapy successfully.
FAQs About Naltrexone Side Effects
How can I stop nausea from naltrexone?
To alleviate nausea from naltrexone, consider taking the medication with food, staying well-hydrated, and possibly adjusting the timing of your doses. Implementing these strategies may significantly improve your experience.
Can naltrexone cause depression?
Naltrexone may initially cause mood changes, including increased anxiety or depressive symptoms in some individuals; however, consistent use often leads to an improvement in mood over time. It is essential to monitor these effects with a healthcare professional.
Will naltrexone make me gain weight?
Naltrexone is not commonly associated with weight gain. Maintaining a healthy lifestyle is advisable to manage any potential weight changes.
How long do naltrexone side effects last?
Naltrexone side effects typically resolve within a few days to weeks as your body adjusts to the medication. However, any persistent or bothersome symptoms should be discussed with a healthcare provider.
When should I stop taking naltrexone due to side effects?
You should stop taking naltrexone immediately if you experience severe side effects such as liver dysfunction, allergic reactions, or significant psychological symptoms, and consult with a healthcare provider.















