Naloxone is a medication that reverses opioid overdoses by restoring normal breathing. It binds to opioid receptors in the brain, making it a critical tool in emergency situations. In this article, you’ll learn “what is naloxone,” how it works, and its various uses.
Key Takeaways
- Naloxone is an opioid antagonist that reverses the life-threatening effects of opioid overdoses by rapidly displacing opioids from brain receptors, restoring normal breathing and consciousness.
- FDA-approved formulations, including injectable versions and over-the-counter nasal sprays, enhance public access to naloxone, making it easier for both healthcare professionals and laypersons to administer in emergencies.
- While naloxone is effective for opioid overdoses, it has limitations, including a shorter duration of action and ineffectiveness against non-opioid overdoses, necessitating ongoing medical monitoring.
What is naloxone and how does it work?
Naloxone is an opioid antagonist that binds to opioid receptors in the brain. Naloxone blocks and reverses the effects of opioids like heroin and fentanyl addiction. This makes naloxone invaluable in opioid overdose cases, restoring breathing and consciousness.
During an opioid overdose, breathing may slow or stop due to the sedative effects. Naloxone swiftly displaces opioids from brain receptors, reversing life-threatening effects and restoring normal breathing. It acts like a reset button, providing a critical window to seek further medical attention.
FDA-approved naloxone formulations
Several FDA-approved formulations of naloxone ensure accessibility and ease of administration. These include injectable versions and prepackaged nasal sprays. Injectable naloxone, like Zimhi, comes in single-dose prefilled syringes for muscle injection. Healthcare professionals and first responders often use this format for its rapid action and reliability.
Nasal sprays like Narcan and RiVive are more user-friendly for laypersons. Narcan, the first over-the-counter naloxone nasal spray, contains 4 mg of naloxone hydrochloride and is designed for easy use, even in high-stress situations. This ease of use is critical for bystanders who may need to administer naloxone quickly during a suspected overdose.
These OTC formulations enhance public access, combating the opioid overdose crisis.
How naloxone reverses opioid overdose
Naloxone quickly restores normal breathing in opioid overdose cases. It displaces opioids from the brain’s μ-receptors, reversing respiratory depression. This rapid displacement reverses overdose symptoms within minutes, restoring breathing and consciousness.
Naloxone’s effects last 30 to 90 minutes, often shorter than some opioids’ duration in the body. Additional doses may be required if opioids like those involved in a suboxone overdose remain active after the initial dose wears off.
Continuous medical monitoring ensures stability until the opioids are fully metabolized.
What is naloxone used for in clinical and public settings?
Naloxone is primarily used for emergency opioid overdose reversal, making it essential in clinical and public settings. Healthcare professionals administer naloxone in clinical settings as part of standard emergency protocols. In public settings, bystanders, family members, or friends often use naloxone for those at risk.
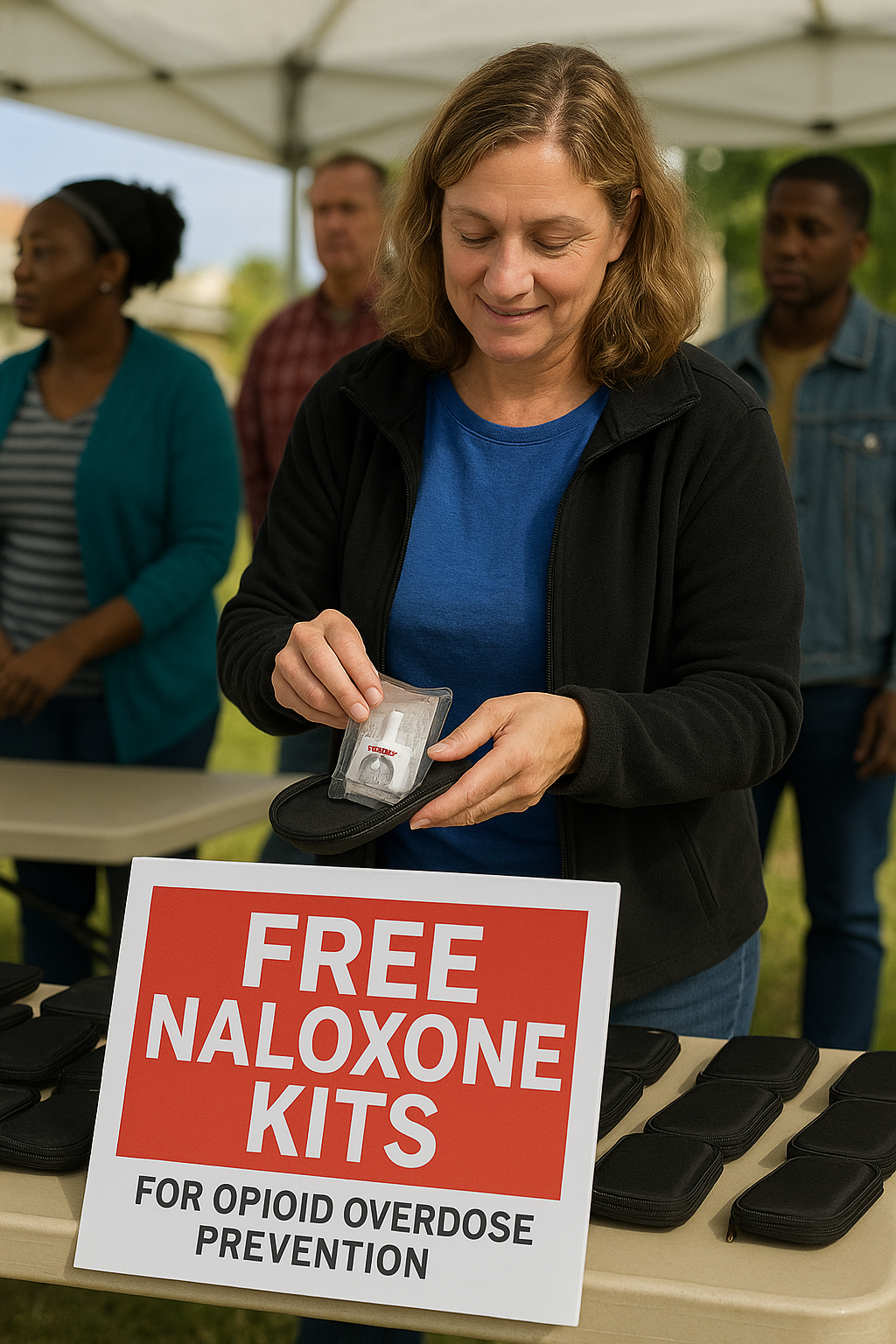
Widespread naloxone distribution of naloxone kits and take-home naloxone (THN) programs has significantly increased its availability, enabling more people to carry and use it during emergencies. These initiatives aim to reduce fatal overdoses through timely intervention and crucial education on recognizing and responding to overdoses.
Emergency medical response
In emergency medical situations, naloxone is crucial for treating suspected opioid overdoses. EMS and hospitals use naloxone to revive individuals experiencing overdose symptoms like shallow breathing or loss of consciousness. For example, 66.1% of individuals resuscitated by EMS for opioid overdose in Rhode Island received naloxone, highlighting its importance in emergency care.
Recognizing overdose symptoms is crucial for effective treatment. First responders are trained to identify signs like pinpoint pupils, shallow breathing, and unresponsiveness. Administering naloxone can be life-saving, but emergency medical care is crucial to ensure safety once it wears off.
Community distribution and take-home kits
Public health initiatives have increased naloxone accessibility for at-risk individuals and caregivers through community distribution and take-home kits. Programs like those from SAMHSA distribute naloxone kits to high-risk individuals, family members, and friends who might witness an overdose.
These initiatives effectively reduce overdose fatalities. For example, a quality improvement project at Burnaby Hospital aimed to increase THN kit distribution from 51% to over 80% for eligible patients, which could potentially save lives. Education and standardized ordering in medical settings ensure healthcare providers consistently consider giving these lifesaving kits to patients before discharge.
Naloxone vs naltrexone: What’s the difference?
Both naloxone and naltrexone combat opioid-related issues but serve different purposes. Naloxone is used for treating opioid overdoses, providing a rapid response to reverse life-threatening symptoms. Naltrexone, however, is used for long-term management of opioid and alcohol dependence, preventing relapse rather than treating an active overdose.
Understanding these medications’ differences is crucial for effective treatment and harm reduction. Naloxone’s immediate effects make it suitable for emergencies, while both naltrexone vs suboxone serve longer-term roles in addiction recovery treatment.
Key differences in use and effect
Naloxone’s effects are immediate and temporary, lasting 30 to 90 minutes, designed to quickly reverse overdose symptoms. Naltrexone, in contrast, blocks opioid effects for over 24 hours, aiding in relapse prevention for those recovering from opioid addiction.
Naloxone can be administered without a prescription in emergencies, while naltrexone requires a prescription and is part of a structured treatment plan. Naltrexone can be taken as a daily pill or monthly injection, making it suitable for ongoing treatment, unlike naloxone, which is used solely in emergencies.
Who should carry naloxone and when should it be used?
The CDC and state health departments recommend that anyone at risk for opioid addiction, including those with opioid use disorder, carry naloxone. This recommendation includes family members, friends, and caregivers who might witness an overdose, as well as healthcare providers who can administer naloxone during an emergency.
Carrying naloxone is vital for individuals at high risk of overdose, like those on high-dose opioid medications or with a history of substance use disorders. Having naloxone readily available can provide life-saving naloxone during an opioid emergency.
Risk factors for needing naloxone
Several risk factors increase opioid overdose likelihood, making naloxone access essential for at-risk individuals. These include:
- Taking high-dose opioid medications, especially those prescribed 50 morphine milligram equivalents or more per day.
- Combining opioids with benzodiazepines.
- Combining opioids with other depressants like alcohol, which significantly heightens overdosing risk.
The presence of potent synthetic opioids like fentanyl in the drug supply also increases the risk of fatal overdoses. Individuals with a history of previous overdoses or chronic health conditions like heart disease or respiratory disorders are also at higher risk and should carry naloxone.

Naloxone side effects and safety considerations
Naloxone is generally considered safe with rare adverse effects. Allergic responses are rare. The primary concern when administering naloxone is the potential for withdrawal symptoms in opioid-dependent individuals, which can vary based on their opioid withdrawal symptoms timeline but are typically not life-threatening.
Despite these considerations, naloxone is effective only for opioid overdoses and will not cause harm if given to someone not experiencing an opioid overdose. This makes it crucial in harm reduction strategies, as it can be safely administered to individuals of all ages.
Is naloxone dangerous to administer?
Administering naloxone is safe and can be given to individuals, even those who may have unknowingly ingested opioids. While it can cause withdrawal symptoms like sweating, nausea, and rapid heart rate in opioid-dependent individuals, these symptoms are rarely life-threatening.
Emergency medical assistance should always be sought after administering naloxone, as its effects last only 30 to 90 minutes. This ensures that any renewed overdose symptoms can be managed effectively once naloxone wears off, and emergency treatment is available if needed.
How to administer naloxone (step-by-step)
Administering naloxone is straightforward, especially with nasal spray formulations. To use a naloxone nasal spray:
- Lay the patient on their back with their neck supported.
- Hold the nasal spray with your thumb on the bottom and fingers on the sides.
- Insert the nozzle into one nostril.
- Press the plunger to deliver the dose.
- After administering the dose, monitor the patient closely.
- Place the patient on their side to maintain an open airway.
If the patient does not respond, naloxone can be repeated every 2 to 3 minutes until they show signs of recovery or emergency help arrives. It is crucial to call 911 or seek emergency medical help immediately after administering naloxone to ensure the person receives comprehensive care.
Naloxone dosage and repeat use
The standard initial dose of naloxone for adults is typically 3 to 8 milligrams, administered as one spray into a nostril. For nasal administration, it is advised to alternate nostrils for each subsequent dose to enhance effectiveness. Some opioid medications, especially those like buprenorphine, may require higher doses of naloxone for effective reversal.
In cases where the initial dose does not elicit a response, additional doses can be administered every 2 to 3 minutes until the individual starts to recover or emergency assistance arrives. Two doses of naloxone’s reversal effects are temporary, making it essential to monitor the patient until the opioids are fully metabolized.
Is naloxone available over the counter?
Naloxone is available over the counter in most states without a prescription. This accessibility allows individuals to purchase naloxone from local pharmacies, online retailers, and community programs. The availability of over-the-counter naloxone aims to increase access to naloxone, this life-saving medication, ensuring that more people can carry it and be prepared to use it during an opioid emergency.
The FDA’s approval of over-the-counter naloxone formulations like Narcan nasal spray has made it easier for the public to obtain naloxone without needing a prescription, further supporting efforts to combat the opioid overdose crisis.
Cost and insurance coverage
The cost of naloxone can vary significantly between over-the-counter purchases and prescription options. Over-the-counter naloxone, such as Narcan nasal spray, might be more expensive than prescription versions. However, many insurance plans, including Medicaid, often cover the cost of naloxone when prescribed, making it more affordable for individuals who need it.
For those without insurance, community programs and health departments sometimes provide free kit naloxone kits to ensure that cost does not become a barrier to accessing this life-saving medication. It’s essential to check with local pharmacies and healthcare providers about the availability and cost of naloxone in your area.
Legal protections for naloxone use
Legal protections for naloxone use are crucial to encourage bystanders to administer the medication during an opioid emergency without fear of legal repercussions. Good Samaritan laws, enacted in 35 states, protect individuals from prosecution for minor drug offenses when they seek emergency help during an overdose. These laws aim to reduce the hesitation in giving naloxone and calling for help.
Additionally, third-party prescribing laws allow healthcare providers to prescribe naloxone to individuals who are not their patients but may assist someone at risk of an overdose. Standing order laws enable pharmacists and certain other personnel to dispense naloxone without requiring a prescription, further increasing accessibility.
Limitations of naloxone
While naloxone is highly effective in reversing opioid overdoses, it does have limitations. Its effectiveness can be influenced by the characteristics of the opioid involved, particularly with long-acting opioids that have a strong affinity for the μ-opioid receptor. Certain synthetic opioids may require higher or additional doses of naloxone to achieve the desired reversal effect.
Naloxone is only effective for opioid overdoses and does not reverse overdoses from other substances such as cocaine or methamphetamine. Furthermore, the effects of naloxone last for approximately 30 to 90 minutes, which might be shorter than the duration of some opioids in the body, necessitating ongoing medical monitoring and additional doses.
Bottom Line: What is Naloxone
Naloxone is a vital tool in the fight against the opioid overdose crisis. As an opioid antagonist, it provides an immediate and effective response to opioid overdoses, restoring normal breathing and consciousness. Available in various formulations, including nasal sprays and injectables, naloxone is accessible to both healthcare professionals and the general public.
By understanding who should carry naloxone, how to administer it, and its safety profile, we can be better prepared to respond to opioid emergencies. While naloxone has its limitations and does not address non-opioid overdoses, its role in harm reduction and saving lives is undeniable. Equipped with this knowledge, we can take proactive steps to provide naloxone, support those at risk, and ultimately, save lives.
FAQs about naloxone
Can naloxone be used more than once?
Yes, naloxone can be used more than once; additional doses can be administered every 2 to 3 minutes if there is no response or if overdose symptoms return.
Does naloxone work for fentanyl?
Naloxone is effective in reversing fentanyl overdoses, but higher or additional doses may be necessary due to fentanyl's potency. It's crucial to be prepared for this possibility in overdose situations.
How long does naloxone last in the body?
Naloxone typically lasts in the body for about 30 to 90 minutes, which may be shorter than some opioids. Therefore, it's important to be prepared for the possibility of needing additional doses.
Is naloxone safe for children?
Naloxone is safe for children and can be administered without risk, even if they are not experiencing an opioid overdose. It's important to ensure that the medication is accessible in emergency situations.
Where can I get naloxone?
You can obtain naloxone over the counter at most pharmacies, as well as through online retailers and community programs. Additionally, local health departments and organizations may offer free naloxone kits to those in need.
















