Looking to manage opiate withdrawal? Detox medications for opiates can make the process safer and more bearable. This article covers the top medications and how they support recovery.
Key Takeaways
- Detox medications, including methadone, buprenorphine, clonidine, and naltrexone, significantly alleviate withdrawal symptoms and help manage opioid use disorder.
- The choice of detox medication should be tailored to individual patient needs, considering factors such as addiction severity, medical history, and the detoxification setting.
- While detox medications provide essential support for managing opiate withdrawal, they carry risks such as dependency and misuse, necessitating careful medical supervision during detoxification.
Introduction to Detox Medications for Opiates
Opiate detoxification involves eliminating opioid drugs from the body, a necessary step for overcoming opioid use disorder. This process can be highly uncomfortable and even dangerous without proper medical intervention. Detox medications help manage withdrawal symptoms, making detoxification safer and more manageable. The use of an opioid drug can complicate this process.
Several medications are commonly used in the detoxification process. These include:
- Methadone
- Buprenorphine
- Clonidine
- Naltrexone
Each of these medications has unique properties and functions, which we will explore in detail in the following sections.

Types of Detox Medications for Opiates
Detox medications significantly alleviate the discomfort associated with prescription opioid withdrawal, supporting recovery by reducing symptoms and cravings to treat pain, prevent withdrawal symptoms and avoid withdrawal symptoms, providing pain relief and addressing disorder opioid with opioid medications to control pain. Understanding how opioids work can further enhance treatment strategies.
Here are the four primary types of detox medications: methadone, buprenorphine, clonidine, and naltrexone.
Methadone
Methadone is widely used in both detoxification and long-term maintenance treatment of opioid dependence, often compared to Suboxone in Suboxone vs methadone treatment strategies. As a full opioid agonist, it activates opioid receptors in the brain, alleviating withdrawal symptoms and reducing cravings. While effective, it carries risks such as potential misuse and dependency.
Methadone is typically administered on a tapered schedule, gradually reducing the dosage over time to minimize withdrawal symptoms and help patients wean off the drug.
Buprenorphine
Buprenorphine, a partial opioid agonist, is widely used for detoxification and treating opioid dependence. Unlike full agonists, it activates opioid receptors to a lesser extent, easing withdrawal symptoms and reducing cravings. Its lower potential for misuse compared to methadone is a significant benefit.
Buprenorphine is often combined with naloxone, an opioid antagonist, to form Suboxone — a key comparison in Suboxone vs methadone treatment approaches — to further reduce misuse risk. It can be administered in various forms, making it a flexible option for treating opioid addiction.
Clonidine
Clonidine, a non-opioid medication, alleviates withdrawal symptoms like anxiety, agitation, and high blood pressure by lowering blood pressure and reducing the body’s fight-or-flight response. While it significantly relieves physical symptoms, it does not address opioid cravings.
Despite its limitations, clonidine remains valuable in detoxification, particularly when combined with other treatments for comprehensive care.
Naltrexone
Naltrexone is used post-detox to prevent relapse by blocking the effects of opioids, thereby reducing cravings. It is effective in maintaining long-term sobriety but must be used cautiously, as it can induce withdrawal symptoms if opioids are present in the system.
Naltrexone’s advantages include reducing cravings and preventing relapse, but potential drawbacks like the risk of precipitated withdrawal must be managed carefully.

How Detox Medications Work for Opiates
Detox medications for opiates or opioids interact with opioid receptors in the brain, alleviating withdrawal symptoms and making it easier to stop using opioids. Methadone and buprenorphine act on these receptors to reduce cravings and withdrawal, though they provide less intense pleasurable effects compared to other opioid drugs.
Methadone, a full opioid agonist, fully activates opioid receptors, providing significant relief from withdrawal symptoms but carrying a higher risk of dependency. In contrast, buprenorphine, a partial opioid agonist, activates these receptors to a lesser extent, easing withdrawal symptoms while posing a lower risk of misuse.
Naltrexone blocks opioid receptors, preventing the euphoric effects of opioids and reducing cravings. These different mechanisms explain why some medications are used during detox, while others like naltrexone are utilized post-detox to maintain sobriety.
The Role of Detox Medications in Opiate Withdrawal Treatment
Detox medications are crucial for alleviating the intense discomfort of opiate withdrawal. They manage symptoms, making the detox process more bearable and safer.
Managing Withdrawal Symptoms
Opiate withdrawal symptoms can be severe, including nausea, sweating, muscle aches, and anxiety, making the detoxification process extremely challenging and increasing the risk of relapse if not properly managed.
Detox medications ease these symptoms. Buprenorphine can significantly reduce withdrawal severity, helping individuals stay committed to detox. Clonidine alleviates physical symptoms like anxiety and sweating, providing relief during this challenging time.
Duration of Treatment
The duration of detox medication usage varies based on the patient’s response and level of dependence. Some may need medication for only a few days, while others require weeks of treatment to manage withdrawal symptoms fully.
When short-term detoxification does not fully address a patient’s needs, transitioning to long-term maintenance therapy may be necessary. This approach ensures sustained recovery and reduces the risk of relapse, offering a comprehensive solution to opioid addiction.

Benefits and Risks of Detox Medications for Opiates
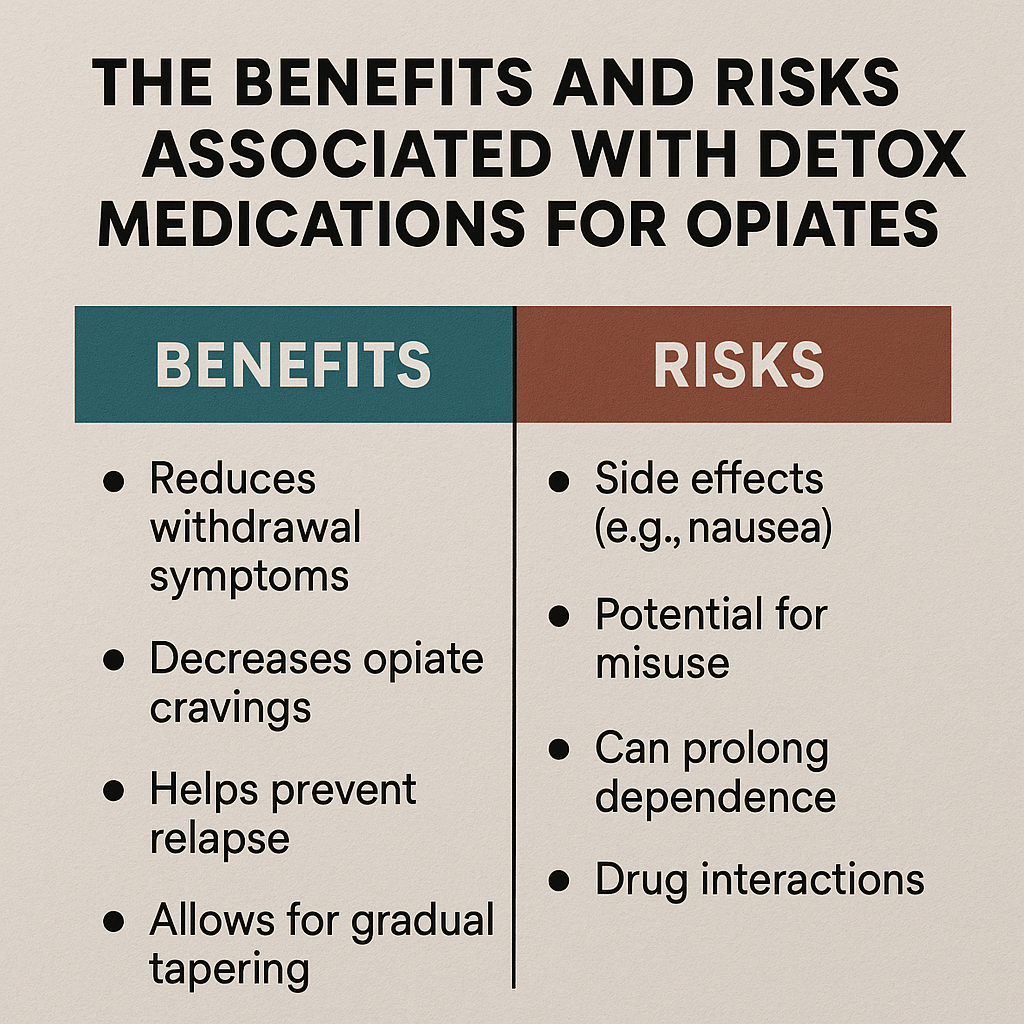
Detox medications offer numerous benefits in managing opiate withdrawal but also come with potential risks that need careful consideration, including the use of hydrocodone vicodin.
Benefits
A primary benefit of detox medications is the safe management of withdrawal symptoms. They significantly reduce physical and psychological discomfort, making the detox process more tolerable and increasing the likelihood of successful recovery.
Detox medications also reduce the risk of relapse during detoxification. By alleviating withdrawal symptoms and cravings, they provide a smoother transition away from opioid dependence, improving patient comfort and outcomes.
Risks
Despite their benefits, detox medications have risks. There is a potential for physical dependence, particularly with methadone and buprenorphine. Misuse of medications like methadone can lead to serious side effects, including sedation and respiratory depression.
Another risk is to develop tolerance, where higher doses are needed over time to achieve the same effect. Abruptly stopping detox medications can cause withdrawal symptoms, highlighting the need for proper medical supervision during detox.
Alternatives to Detox Medications for Opiates
Though highly effective, some individuals may prefer or find alternative methods beneficial alongside medication-assisted treatment.
Natural Detox
Natural detox methods, such as hydration, exercise, and proper nutrition, support the body’s recovery during detoxification. These methods help alleviate some withdrawal symptoms and promote overall well-being with the aid of natural substances.
However, natural detox methods have limitations and may not effectively manage severe withdrawal symptoms. Medical detox is often preferred for individuals with significant opioid dependence to ensure the process is safe and any complications are promptly addressed.
Behavioral Therapy and Support
Behavioral therapy and support are crucial in detoxification. Counseling and therapy, especially cognitive-behavioral therapy (CBT), address the psychological aspects of addiction and equip individuals with coping strategies to manage cravings and prevent relapse related to substance abuse.
Group therapy provides social support, allowing individuals to share experiences and support one another in recovery. This shared experience enhances motivation and fosters a sense of community, essential for sustained recovery.
Special Considerations in Choosing Detox Medications
Choosing the right detox medication requires considering the patient’s unique circumstances, including their medical history, addiction severity, and any co-occurring health conditions.
Patient-Specific Factors
Detox medication choices must be tailored to each patient’s needs. Factors like opioid use patterns, underlying health conditions, and medical history determine the most appropriate medication. For example, pregnant women, individuals with liver or kidney issues, or those with a history of mental health disorders may require special considerations.
A personalized approach ensures the chosen detox medication is safe and effective, minimizing risks and maximizing the chances of successful detoxification.
Detox in Inpatient vs. Outpatient Settings
The detoxification setting significantly impacts its success. Inpatient detox programs offer constant medical supervision and a structured environment, crucial for individuals with severe withdrawal symptoms or those at high risk of relapse.
Outpatient detox programs provide more flexibility and are less intensive, suitable for individuals with milder withdrawal symptoms and strong support systems at home.
Both settings have advantages, and the choice should be based on the patient’s specific needs and circumstances.
The Future of Detox Medications for Opiates
The future of detox medications for opiates is promising, with ongoing research developing opioid treatments to improve outcomes for individuals with opioid use disorder and the opium poppy.
Advances in Medication-Assisted Treatment (MAT)
Emerging MAT strategies focus on personalized medicine to better cater to individual patient needs and improve treatment effectiveness. Recent advancements include novel formulations of existing medications that enhance effectiveness and reduce misuse potential.
Regulatory changes have made it easier for practitioners to prescribe buprenorphine, increasing access to this life-saving medication. Growing evidence indicates that MAT significantly reduces overdose deaths for individuals using methadone or buprenorphine, underscoring the importance of these treatments in combating the opioid crisis.
Bottom Line: Detox Medications for Opiates
Detox medications are a cornerstone in treating opioid withdrawal, providing essential support to manage symptoms and reduce relapse risk. Medical supervision and a comprehensive, multi-faceted approach, including medically supervised withdrawal, are crucial for safe and effective detoxification.
Seeking professional help is vital to ensure the best outcomes and pave the way to recovery through mental health services.
FAQs About Top Detox Medications for Opiates
What are the main types of detox medications used for opiates?
The primary detox medications for opiates are methadone, buprenorphine, clonidine, and naltrexone. Each of these plays a significant role in managing withdrawal symptoms and aiding recovery.
How does methadone work in opiate detox?
Methadone effectively alleviates withdrawal symptoms during opiate detox by activating opioid receptors as a full opioid agonist. This mechanism provides necessary support for individuals undergoing treatment, facilitating a smoother transition.
What are the benefits of using buprenorphine for detox?
Using buprenorphine for detox offers the significant benefit of a lower potential for misuse while effectively easing withdrawal symptoms and cravings. This makes it a safer and more manageable option during the detoxification process.
What role does clonidine play in detox?
Clonidine plays a supportive role in detox by alleviating withdrawal symptoms such as anxiety and high blood pressure, while not addressing cravings directly. Its use can facilitate a more comfortable withdrawal experience for patients.
How does naltrexone help prevent relapse after detox?
Naltrexone effectively prevents relapse after detox by blocking the effects of opioids, thereby reducing cravings for these substances. This helps individuals maintain their recovery by diminishing the urge to use.
















