Choosing between Methadone vs Buprenorphine for opioid addiction treatment can be challenging. This article breaks down their differences, effectiveness, and who they are best suited for, helping you make an informed choice.
Key Takeaways
- Methadone is generally more effective than buprenorphine in retaining patients in treatment programs, especially for those with severe opioid dependence.
- Buprenorphine, as a partial agonist, offers a lower risk of overdose and can be prescribed for home use, making it a convenient option for patients with mild to moderate opioid dependence.
- The choice between methadone and buprenorphine should be individualized based on patient needs, treatment goals, and potential risks, with guidelines recommending both for opioid addiction treatment.
Which is more effective: methadone or buprenorphine?
When it comes to treating opioid addiction:
- Methadone has been shown to be more effective than buprenorphine in maintaining patients in treatment programs.
- Studies indicate that methadone treatment results in higher retention rates, which is crucial for long-term recovery.
- Buprenorphine is effective in suppressing illicit opioid use for those who remain in treatment.
- However, buprenorphine does not consistently match methadone in keeping patients engaged.
However, the effectiveness of both medications can vary based on individual patient factors and the specific context of their use. For patients with mild to moderate opioid dependence, buprenorphine may be a suitable option, while methadone is generally preferred for those with higher levels of dependence. Clinical guidelines recommend both methadone and buprenorphine as first-line treatments for opioid dependence, considering individual patient needs.
Ultimately, the choice between methadone and buprenorphine should be guided by clinical evaluations and patient preferences. Both medications offer a pathway to recovery, but the journey’s success largely depends on the individual’s circumstances and the support they receive throughout their treatment.

Key differences between methadone and buprenorphine
Understanding the key differences between methadone and buprenorphine is essential for making an informed decision. Here’s a side-by-side comparison:
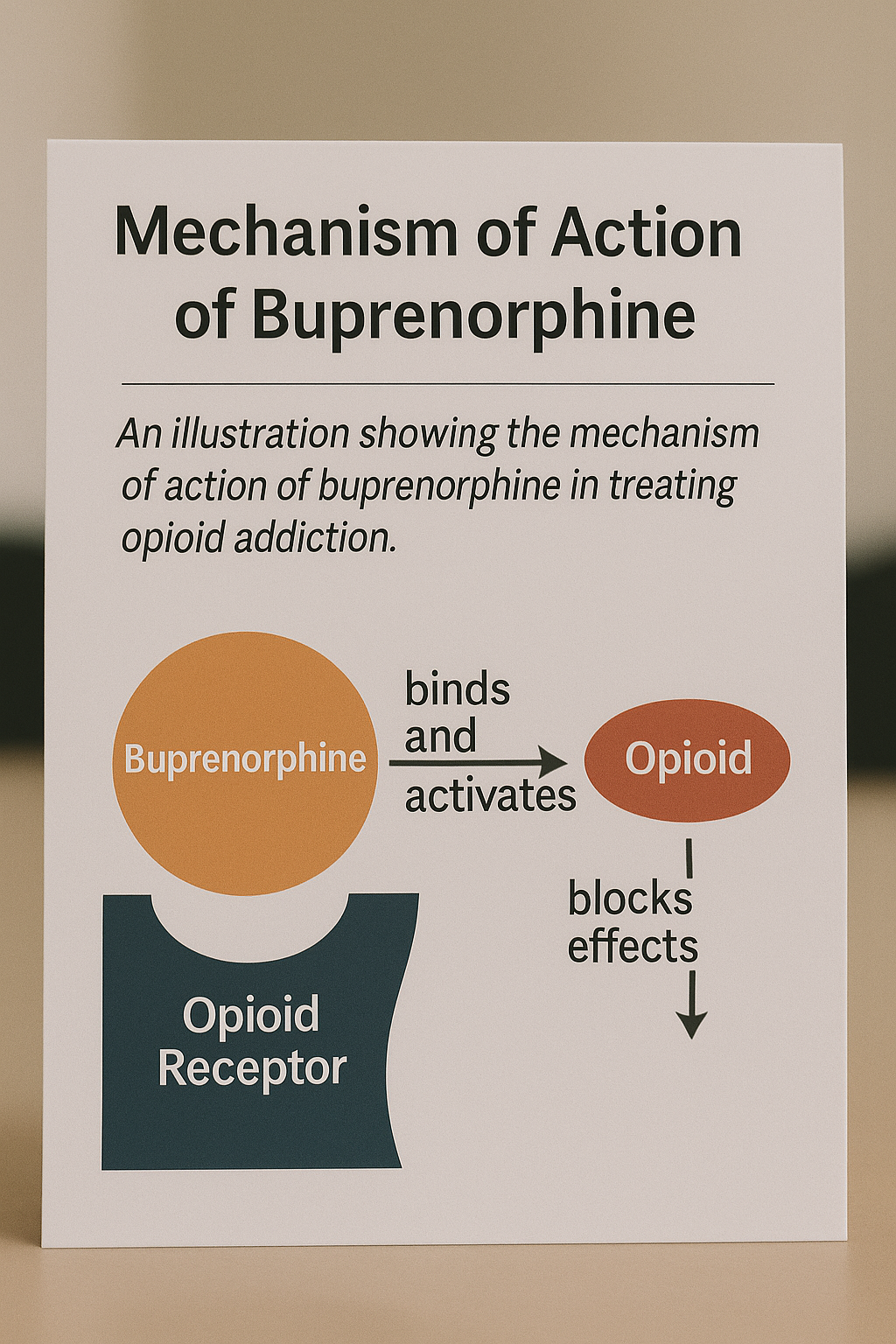
- Mechanism of Action:
- Methadone: Full opioid agonist that activates opioid receptors fully, leading to a higher potential for overdose.
- Buprenorphine: Partial opioid agonist that only partially activates the receptors, reducing the risk of overdose.
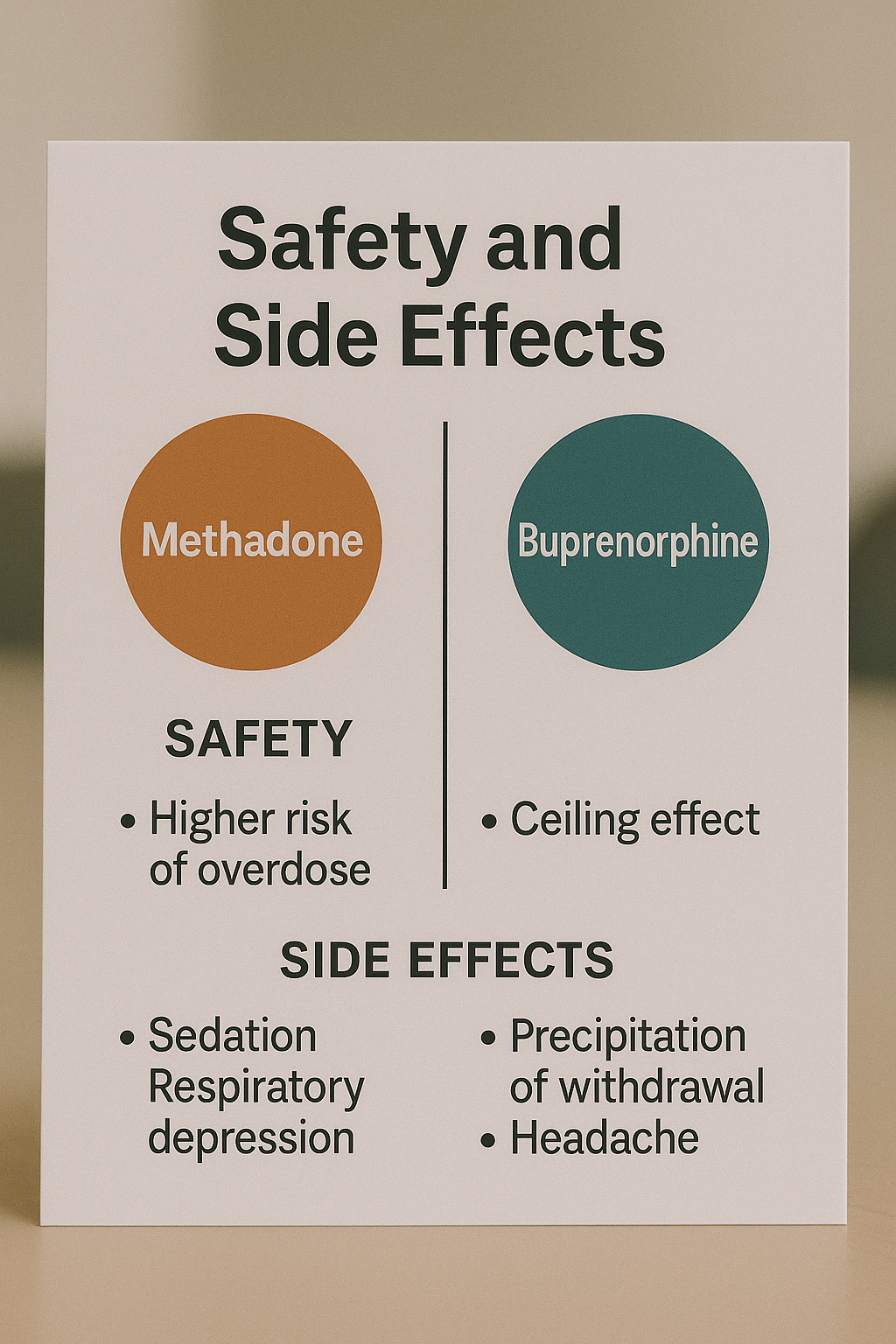
- Potency:
- Methadone: More potent with no ceiling effect, which means its effects increase with dosage.
- Buprenorphine: Has a ceiling effect that limits its effects at higher doses, making it safer in terms of overdose risk.
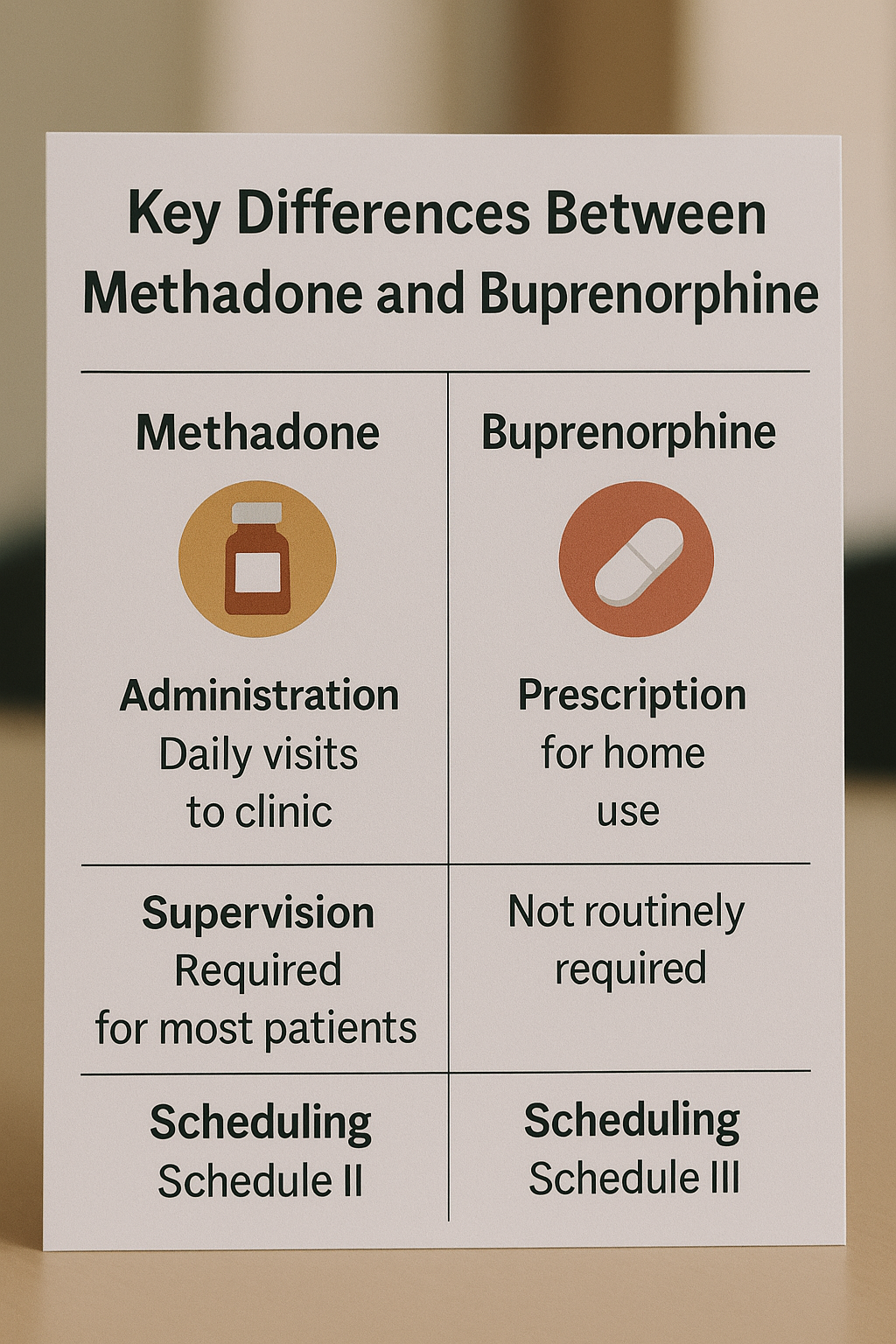
- Administration:
- Methadone: Typically administered in liquid form under supervision at a methadone clinic.
- Buprenorphine: Often prescribed in tablet form, allowing for easier at-home use but posing challenges for monitoring.
- Cost:
- Methadone: Generally cheaper but involves more frequent healthcare visits.
- Buprenorphine: Higher medication costs but fewer healthcare visits, which can balance overall expenses.
- Safety:
- Methadone: Higher risk of overdose and respiratory depression.
- Buprenorphine: Lower risk of respiratory depression and overdose due to its ceiling effect.
These significant differences highlight that while both two medications are effective, patients may also want to compare Suboxone vs Methadone to understand formulation-specific factors that affect daily use. Patients should consider these factors in consultation with their healthcare providers to determine the best course of action.
What is methadone?
Methadone is a synthetic opioid used primarily to manage opioid dependence and alleviate withdrawal symptoms from heroin and other opioids. As a full opioid agonist, methadone activates the same receptors in the brain as other opioids, but it does so in a controlled manner to reduce cravings and withdrawal symptoms without producing the intense high associated with drugs like heroin. Common brand names for methadone include Methadose and Dolophine.
Methadone has been a cornerstone of opioid addiction medicine treatment for decades. Its long history of use and effectiveness in reducing opioid cravings make it a trusted option in many addiction treatment programs. However, its use requires careful monitoring due to the potential for misuse and overdose, especially in the context of addict med.
Methadone treatment typically involves daily administration at certified opioid treatment programs (OTPs), where patients receive their doses under supervision to ensure compliance and reduce the risk of diversion.
How methadone works
Methadone acts on the same brain receptors as other opioids, but it does so in a way that mitigates cravings without producing a euphoric high. This is achieved by stabilizing brain chemistry and altering the brain’s response to pain, which helps alleviate withdrawal symptoms.
A single dose of methadone can last between 24 to 36 hours, providing a controlled release that prevents rapid dopamine spikes. This long-acting nature makes it effective for daily management of opioid dependence, reducing cravings and blocking the euphoric effects of other opioids.
Methadone primarily operates as a full agonist at the mu-opioid receptors, leading to a significant reduction in withdrawal symptoms and cravings. This makes it an essential component of comprehensive opioid addiction treatment programs.
Methadone pros and cons
Methadone offers several benefits, including:
- A long history of use
- Powerful symptom relief
- Effective diminishment of cravings for other opioids
- A less intense experience compared to drugs like heroin
- A structured routine of daily visits for administration that fosters accountability in recovery.
However, there are drawbacks to methadone treatment:
- It can lead to physical dependence.
- It has a higher risk of overdose compared to other treatments.
- The stigma associated with methadone clinics can discourage patients from seeking care.
- The perception of restricted access can also discourage patients from seeking necessary care.
Patients may experience several side effects from methadone, including respiratory issues and potential dental problems due to sugar content. Despite these challenges, methadone remains a viable option for many individuals struggling with severe opioid dependence.
What is buprenorphine?
Buprenorphine is a prescription opioid used primarily for treating opioid dependence and sometimes severe pain. As a partial opioid agonist, it provides some opioid effects while having a lower risk of misuse and overdose compared to full agonists. Key formulations of buprenorphine include:
- Suboxone (buprenorphine + naloxone)
- Subutex
- Sublocade
- Probuphine.
Buprenorphine’s unique properties make it an effective option for opioid addiction treatment. Its ability to mitigate withdrawal symptoms and reduce cravings helps individuals transition to sobriety. The various formulations offer flexibility in administration, catering to different patient needs.
Unlike methadone, buprenorphine can be prescribed for home use, making it a more convenient option for many patients. This flexibility, combined with its safety profile, has made buprenorphine a popular choice in opioid addiction treatment programs.
How buprenorphine works
Buprenorphine functions as a partial agonist at the mu opioid receptor, meaning it only partially activates the receptors, which reduces the risk of misuse and overdose compared to full agonists. This ceiling effect limits its effects at higher doses, making it safer in terms of respiratory depression.
Buprenorphine mitigates pain by interfering with pain signaling in the nervous system and helps ease withdrawal symptoms when replacing other opioids. Its high affinity for opioid receptors means it can block the effects of other opioids, which is beneficial for patients transitioning from stronger opioid medications to reduce pain and manage pain management and opioid withdrawal symptoms.
The drug’s long-acting nature allows for less frequent dosing, with some patients not requiring daily administration. This flexibility makes buprenorphine an attractive option for many individuals seeking long term treatment for opioid dependence.
Buprenorphine pros and cons
Buprenorphine offers several benefits, including office-based prescribing, lower overdose risk, and fewer side effects, especially for patients on long-term use of buprenorphine. Buprenorphine patients undergoing buprenorphine treatment often report an improvement in their overall quality of life, avoiding the negative consequences of drug use.
However, there are limitations to buprenorphine treatment. The partial agonist ceiling means that it may not be as effective for individuals with severe opioid dependence. Additionally, there is a risk of misuse, particularly when combined with other central nervous system depressants. An opioid partial agonist may not be suitable for everyone.
Access to buprenorphine may be limited geographically, often requiring specialized treatment programs. Despite these challenges, buprenorphine remains a viable option for many individuals seeking to overcome opioid addiction.
Safety and side effects: Methadone vs buprenorphine
When comparing the safety and side effects of methadone and buprenorphine, several factors come into play. Buprenorphine poses a lower risk of respiratory depression compared to methadone, largely due to its ceiling effect. However, it can still lead to overdose risks when combined with other depressants like alcohol.
Methadone has been associated with serious cardiac issues, such as Torsades de Pointes, particularly at higher doses. Additionally, the diversion and misuse of buprenorphine are major concerns, especially when it is used intravenously.
In terms of serious adverse events, studies indicate that buprenorphine shows no significant difference compared to methadone compared to methadone. Both medications require careful monitoring and adherence to prescribed guidelines to ensure patient safety and effectiveness in treatment.
Accessibility and regulation
Accessibility and regulation significantly impact the use of methadone and buprenorphine. Regarding methadone treatment:
- It is heavily regulated, requiring dispensing only through certified providers and facilities.
- Initial doses must be taken daily under observation for the first 90 days.
- This daily observed dosing complicates access for patients.
In contrast, buprenorphine can be prescribed more freely, often requiring an X-waiver for physicians. During the COVID pandemic, some methadone regulations were relaxed, allowing for take-home doses and demonstrating that stricter rules may not always be necessary.
Insurance providers are increasingly covering treatments for opioid use disorder, but methadone often involves more regulations compared to buprenorphine, leading to biases in prescribing. The stigma associated with methadone treatment can also discourage patients from seeking care.
Cost comparison of methadone and buprenorphine
The cost of treatment is a crucial factor for many patients. The average treatment cost for the first six months was significantly lower for buprenorphine at approximately $11,597 compared to $14,921 for methadone. Patients undergoing buprenorphine treatment required fewer healthcare visits, averaging 66 visits in the first six months, while methadone patients had 137 visits.
Despite higher medication costs for buprenorphine, overall expenses were comparable to those for methadone due to reduced healthcare utilization. The annual treatment cost for methadone averages around $6,979, while buprenorphine is slightly less expensive at approximately $6,370.
Including criminal justice costs, methadone therapy yields significantly higher lifetime cost savings compared to buprenorphine. When factoring in societal costs, methadone can save an estimated $100,000 per person over a lifetime.
Patient suitability: Who should take methadone or buprenorphine?
Choosing the right treatment options depends on various factors, including:
- The severity of addiction
- Medical history
- Location
- Lifestyle
- Risk tolerance
Patients with severe opioid dependence may benefit more from methadone due to its potency and effectiveness. For those with mild to moderate dependence, an untreated opioid may be a suitable option.
Clear communication between patients and clinicians regarding treatment goals is crucial, as discrepancies often exist between patient expectations and clinical management recommendations. Some patients require more structured support to remain engaged in treatment, while others find the monitoring associated with methadone to be a barrier.
Stigma associated with methadone clinics can lead patients to prefer buprenorphine, which can be taken privately at home. Ultimately, the choice should be guided by a thorough evaluation of the individual’s unique needs and circumstances.
Clinical guidelines and recommendations
Health agencies such as the Substance Abuse and Mental Health Services Administration (SAMHSA), National Institute on Drug Abuse (NIDA), and the World Health Organization (WHO) endorse both methadone and buprenorphine for detoxification and maintenance treatment of opioid dependence. Clinical guidelines recommend methadone for patients with severe opioid dependence due to its high effectiveness. On the other hand, buprenorphine’s ceiling effect makes it a safer alternative, particularly in populations with a high risk of overdose.
The National Institute of Health and Clinical Excellence (NICE) suggests:
- Considering patient preferences when prescribing either medication.
- Emphasizing safety precautions when switching patients from methadone to buprenorphine to avoid precipitated withdrawal syndrome.
- Monitoring liver function for patients prescribed buprenorphine, especially those with a history of intravenous use.
These recommendations highlight the importance of personalized treatment plans that consider the unique needs and circumstances of each patient, ensuring the most effective and safe approach to managing opioid dependence and treating opioid.
Bottom Line: Making the right choice for opioid addiction treatment
Choosing the appropriate treatment for opioid use disorders is crucial for effective recovery and can significantly impact an individual’s health and social functioning. Evidence-based medication-assisted treatment (MAT) approaches, which combine medication with behavioral therapy, have shown to enhance recovery outcomes in individuals with opioid use disorder.
Personalized treatment plans that consider an individual’s unique needs and circumstances can improve the effectiveness of opioid addiction therapies. Support from family and community plays a vital role in the recovery process, helping reduce the stigma associated with opioid use disorder and encouraging individuals to seek the help they need.
FAQs about methadone vs buprenorphine
Can you switch from methadone to buprenorphine?
Yes, you can switch from methadone to buprenorphine, but it must be done under medical supervision to manage the risk of precipitated withdrawal, especially during switching from methadone to Suboxone. A gradual transition is essential for safety and effectiveness.
Is one medication more addictive than the other?
Buprenorphine is generally considered less addictive than methadone because its ceiling effect reduces the risk of misuse. Therefore, while both medications have potential for addiction, buprenorphine may be the safer option.
Which medication has better retention rates?
Methadone demonstrates better retention rates in treatment programs than buprenorphine. This makes it a more effective option for some patients.
Can pregnant women use methadone or buprenorphine?
Pregnant women can use both methadone and buprenorphine safely, although methadone has a more extensive history of use during pregnancy. It is essential to consult a healthcare professional for personalized guidance.
Which medication is more cost-effective?
Buprenorphine is generally considered more cost-effective due to fewer required healthcare visits, despite its higher medication costs. Therefore, the overall expenses may be lower compared to methadone.