Wondering which is more effective for opioid use disorder, Naltrexone vs Buprenorphine? This article will compare their effectiveness, usability, and key differences to help you choose the right treatment.
Key Takeaways
- Buprenorphine is often more effective than naltrexone for treating opioid use disorder due to its ease of initiation during withdrawal, leading to higher patient engagement and lower relapse rates.
- Naltrexone requires patients to be opioid-free for at least seven to ten days before starting treatment, while buprenorphine can be initiated during withdrawal, impacting accessibility and choice of medication.
- Both medications have unique benefits and challenges; buprenorphine carries a risk of misuse due to its partial opioid agonist properties, whereas naltrexone does not have this risk but is less accessible for those still dependent on opioids.
Which is more effective: naltrexone or buprenorphine?
When it comes to treating opioid use disorder, effectiveness is a critical factor. Research indicates that buprenorphine may offer a more effective treatment due to its ease of initiation and adherence among patients. Buprenorphine can be started while the patient is still experiencing withdrawal symptoms, making it more accessible for those in the early stages of treating opioid addiction.
On the other hand, naltrexone requires patients to be completely off opioids for a period before starting treatment, which can hinder its accessibility. Studies have shown that relapses were more frequent among participants using extended-release naltrexone compared to those on buprenorphine. This suggests that while both medications can be effective, the overall likelihood of sustained treatment favors buprenorphine.
However, some studies suggest both medications can be equally effective for those who can successfully start treatment initiation. The challenge lies in the initiation process and patient engagement, where buprenorphine seems to have the upper hand. Ultimately, the choice between naltrexone and buprenorphine depends on individual circumstances and treatment goals.
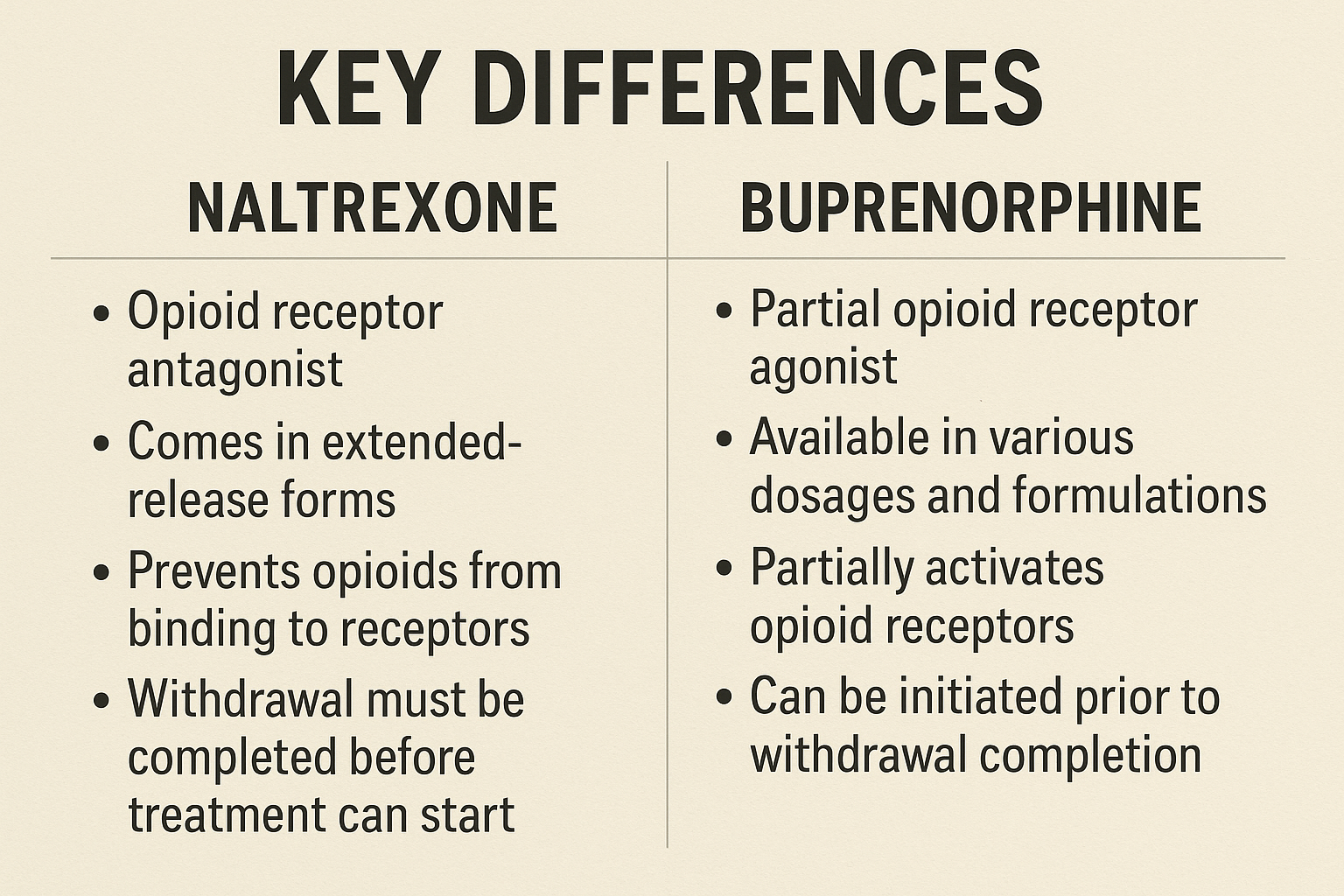
Key differences between naltrexone and buprenorphine
Naltrexone and buprenorphine are both used to treat opioid use disorder, but they function quite differently. Buprenorphine alleviates withdrawal symptoms and cravings by providing a milder opioid effect. In contrast, naltrexone blocks opioid effects completely to curb cravings. This fundamental difference in their mechanisms of action is crucial for understanding their use in the treatment of opioid use.
Another significant difference between buprenorphine and naltrexone includes:
- Buprenorphine can potentially be misused due to its partial opioid effect, whereas naltrexone does not have the same risk of misuse or overdose.
- Naltrexone requires individuals to be opioid-free for at least seven to ten days before starting treatment.
- Buprenorphine can be started during withdrawal, without the need to be opioid-free beforehand.
Both medications have similar adverse effects, including gastrointestinal upset and sleep disturbances. However, the method of administration varies; naltrexone is given as a monthly injection, while buprenorphine is commonly prescribed as a sublingual tablet. Discontinuing naltrexone—commonly known by its brand name Vivitrol- can increase the risk of overdose due to reduced opioid tolerance, which is also a concern when switching between Vivitrol and Suboxone without proper medical oversight.
What is naltrexone?
Naltrexone is a food and drug administration-approved medication used to treat both opioid and alcohol dependency. It is primarily utilized to help individuals overcome opioid addiction by reducing cravings and preventing relapse with FDA approved medications. The drug enforcement administration recognizes naltrexone treatment as an effective option for those seeking recovery.
Naltrexone works as an opioid antagonist, blocking the effects of opioids on the brain.
Mechanism of action
Naltrexone functions by naltrexone binds to opioid receptors in the brain, specifically blocking the mu, kappa, and delta receptors. By doing so, it prevents the euphoric and pain-relieving effects of opioids, making it an effective tool for relapse prevention. The drug’s action as an opioid antagonist means it does not induce a state of euphoria, which is beneficial for individuals recovering from addiction.
Additionally, by blocking these receptors, naltrexone prompts the body to increase endorphin production, which can help alleviate pain and improve mood.
Forms and dosage
Naltrexone is available in two primary forms: a daily pill form and a monthly injectable. The oral naltrexone tablets are typically 50 mg, while the injectable, known as Vivitrol, is administered at 380 mg every four weeks.
The oral form of naltrexone begins to take effect within one hour, whereas the intramuscular injection maintains its therapeutic effects for approximately one month. For those transitioning from other opioids like buprenorphine or methadone, it is essential to consult a healthcare provider to manage potential withdrawal symptoms.
When naltrexone is recommended
Naltrexone is recommended for individuals who have completed opioid withdrawal, typically requiring a 7 to 10 day abstinence period before starting treatment. This makes it suitable for those who have already ceased opioid use and are looking to prevent relapse.
Naltrexone does not cure addiction but should be part of a comprehensive treatment plan that includes therapy and support groups. Monitoring by a healthcare provider is required to ensure its effectiveness and manage any potential side effects.
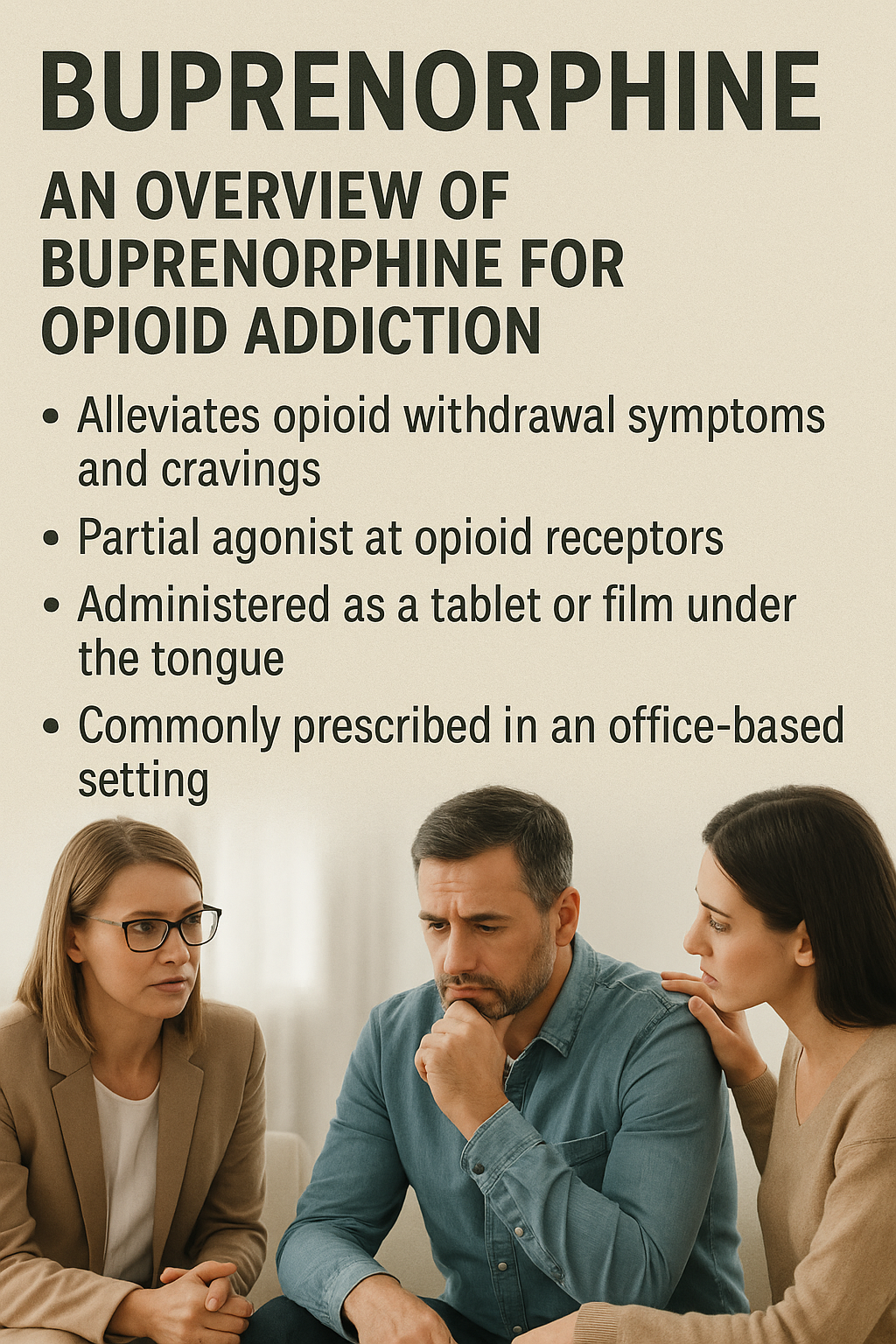
What is buprenorphine?
Buprenorphine is a medication used to treat opioid use disorder, acting as a partial agonist at opioid receptors and is a partial opioid agonist medication. It is commonly known under brand names such as Suboxone and Subutex and plays a crucial role in managing opioid dependence.
Mechanism of action
Buprenorphine binds to opioid receptors in the brain but produces less intense effects compared to full agonists. As a partial agonist at the Opioid Receptor, buprenorphine activates these receptors to a moderate extent, reducing opioid cravings and withdrawal symptoms without causing a full opioid high.
Additionally, buprenorphine acts as a weak antagonist at kappa receptors and an agonist at delta receptors, contributing to its unique pharmacological profile. Its high affinity for mu-opioid receptors results in a prolonged duration of action and a slower onset of withdrawal symptoms, making it a valuable tool in opioid dependence treatment.
Forms and dosage
Buprenorphine is available in various forms, including sublingual buprenorphine tablets and films, with dosages typically ranging from 2 mg to 24 mg. The sublingual form is commonly prescribed for opioid dependence, with the initial dosing often starting at 2 mg to 8 mg.
For maintenance therapy, buprenorphine may be combined with naloxone to prevent misuse. The injectable form is typically used for pain management and can be administered every 6 hours as needed.
When buprenorphine is recommended
Buprenorphine is often recommended for individuals with opioid use disorders who require a long-term management strategy, especially those considering the long-term use of buprenorphine as part of their recovery plan. It is particularly beneficial for those who cannot access methadone facilities or have been on a waitlist for over three months, and healthcare providers may prescribe buprenorphine in these cases. Additionally, those struggling with opioid use disorder (OUD) may find this treatment effective, especially when comparing options like Suboxone vs Methadone to determine what suits their lifestyle and recovery plan.
This medication for opioid use is effective for patients with a limited history of opioid use and those requiring lower doses of opioid agonists. It is also recommended to start buprenorphine during mild-to-moderate opioid withdrawal symptoms to mitigate discomfort.
Pros and cons: naltrexone vs buprenorphine
Each medication has its advantages and disadvantages. Naltrexone, as an opioid antagonist, is less likely to be misused but requires patients to be opioid-free before starting treatment with medication approved for opioid use disorder medications.
Buprenorphine, a partial opioid agonist, can be started during withdrawal but carries a risk of misuse.
Patient experience and adherence
Patient experience and adherence are crucial factors in the success of treatment. Studies indicate that 73% of naltrexone users report a positive effect compared to 57% for buprenorphine. The initiation rate for buprenorphine is higher, reflecting better patient engagement.
Methadone treatment, although effective, has faced significant stigma, impacting patient treatment retention and adherence due to demanding attendance requirements at opioid treatment programs and opioid treatment program (OTPs) and methadone maintenance.
Side effects and risks
Common side effects of buprenorphine include nausea, anxiety, and depression, while naltrexone users often experience nausea and headaches. Naltrexone also has a moderate risk of liver problems, especially when combined with other medications that affect the liver.
Injection site reactions are a concern for naltrexone, while buprenorphine misuse can lead to respiratory depression and opioid overdoses. It is essential for patients to be closely monitored by healthcare providers to manage these risks effectively.
Cost and accessibility of each medication
The cost and accessibility of these medications can significantly impact treatment decisions. Medication-assisted treatment with methadone costs approximately $6,979 per year, while buprenorphine is around $6,370. Extended-release naltrexone is significantly higher at about $15,032 annually.
Insurance coverage and the availability of generic forms can also affect accessibility. Methadone treatment has greater access to healthcare resources, but its availability is limited, impacting effective interventions for opioid use disorder.
Which medication is better for long-term recovery?
Both naltrexone and buprenorphine serve distinct roles in addiction treatment. Naltrexone focuses on supporting abstinence, while buprenorphine assists in maintenance therapy. Naltrexone can help restore the brain’s natural balance post-addiction, whereas buprenorphine maintains opioid-dependent brain function.
Long-term recovery success with naltrexone often relies on strong external support networks, including family and counseling services, especially in cases of substance abuse. Buprenorphine has a ceiling effect, limiting the euphoria users can experience, which helps reduce the risk of misuse during recovery.
Choosing between naltrexone and buprenorphine for long-term recovery is highly individualized and depends on personal circumstances and treatment goals. Both medications can be effective, but the right choice varies from person to person.
Factors to consider when choosing between naltrexone and buprenorphine
When choosing between naltrexone and buprenorphine, several factors must be considered:
- The risk of misuse: naltrexone does not have the potential for abuse, while buprenorphine does.
- The requirement for naltrexone initiation: patients must be opioid-free for at least seven to ten days before starting treatment.
- The patient’s current opioid status can affect the choice of medication.
Buprenorphine can provide relief from withdrawal symptoms and cravings due to its partial agonist properties, influencing treatment decisions for those still dependent on opioids. The method of administration also varies, with naltrexone being an extended-release injection given monthly, while buprenorphine is typically taken as a sublingual tablet.
Patients should also consider potential side effects, as both medications can cause gastrointestinal disturbances and affect sleep. Personal circumstances, such as substance use history, co-occurring abuse and mental health issues, and detox readiness, are critical in making an informed choice.
Bottom Line: Naltrexone vs Buprenorphine
In summary, both naltrexone and buprenorphine offer valuable options for treating opioid use disorder. Naltrexone is an opioid antagonist that requires patients to be opioid-free before starting treatment and is also effective for alcohol dependence. Buprenorphine, a partial opioid agonist, can be started during withdrawal and helps manage cravings and withdrawal symptoms.
Choosing the right medication depends on individual circumstances, including the patient’s current opioid use status, risk of misuse, and personal treatment goals. Both medications are more effective when combined with counseling or therapy, highlighting the importance of a comprehensive treatment approach.
FAQs about Choosing Between Naltrexone and Buprenorphine
Can you switch from buprenorphine to naltrexone?
Switching from buprenorphine to naltrexone is feasible, but it necessitates medical stability and a period of sustained abstinence from opioids to prevent withdrawal symptoms.
Can either naltrexone or buprenorphine be used for alcohol dependence?
Naltrexone is FDA-approved and effective for treating alcohol dependence, whereas buprenorphine is primarily used for opioid use disorder and is not typically recommended for alcohol issues.
Do both medications require counseling or therapy?
Both naltrexone and buprenorphine require counseling or therapy to enhance treatment effectiveness and ensure comprehensive support.
What are the common side effects of buprenorphine and naltrexone?
Buprenorphine commonly causes nausea, anxiety, and depression, while naltrexone may lead to nausea, headaches, and poses a moderate risk of liver issues. It is important to monitor these potential side effects when using either medication.
How do naltrexone and buprenorphine work differently in the brain?
Naltrexone functions as an opioid antagonist, blocking opioid receptors to eliminate euphoric effects, while buprenorphine acts as a partial agonist, mildly activating these receptors to alleviate cravings and withdrawal symptoms. Consequently, their differing mechanisms cater to distinct therapeutic needs in opioid use disorder.
















