Opioid withdrawal occurs when someone who is dependent on opioids stops using them, leading to severe physical and mental symptoms. These symptoms can be life-threatening. In this article, we’ll discuss the stages of withdrawal, what to expect, and why medical supervision is crucial.
Key Takeaways
- Opioid withdrawal occurs when a dependent individual abruptly stops or reduces opioid intake, leading to potentially life-threatening symptoms due to neurochemical changes in the brain.
- Withdrawal symptoms progress through three stages: early-stage (6-24 hours), peak (24-72 hours), and late symptoms (3-7+ days), each with distinct physical and psychological challenges.
- Effective treatment options include medication-assisted treatment (MAT) and supportive care, which together manage symptoms, minimize complications, and support long-term recovery.
What is opioid withdrawal?
Opioid withdrawal is a clinical condition that manifests when someone dependent on opioids abruptly stops or significantly reduces their intake, often leading to opiate withdrawal. This state is not merely uncomfortable but can be life-threatening. Opioids like morphine, heroin, and oxycodone are potent pain relievers, but their use often leads to dependence and addiction. When a person becomes opioid-dependent, their brain’s chemistry and function change, creating a physical and psychological need for the drug.
The sudden cessation of opioids leads to withdrawal symptoms due to a complex interplay of neurochemical factors affecting specific brain areas. These symptoms are the body’s response to the absence of a substance it has grown reliant on, a stark reminder of the opioid epidemic’s socio-economic impact, which includes increased healthcare costs and loss of productivity.
Recognizing this condition is vital for both opioid-dependent patients and their supporters.
How does opioid withdrawal feel and what are the first signs?
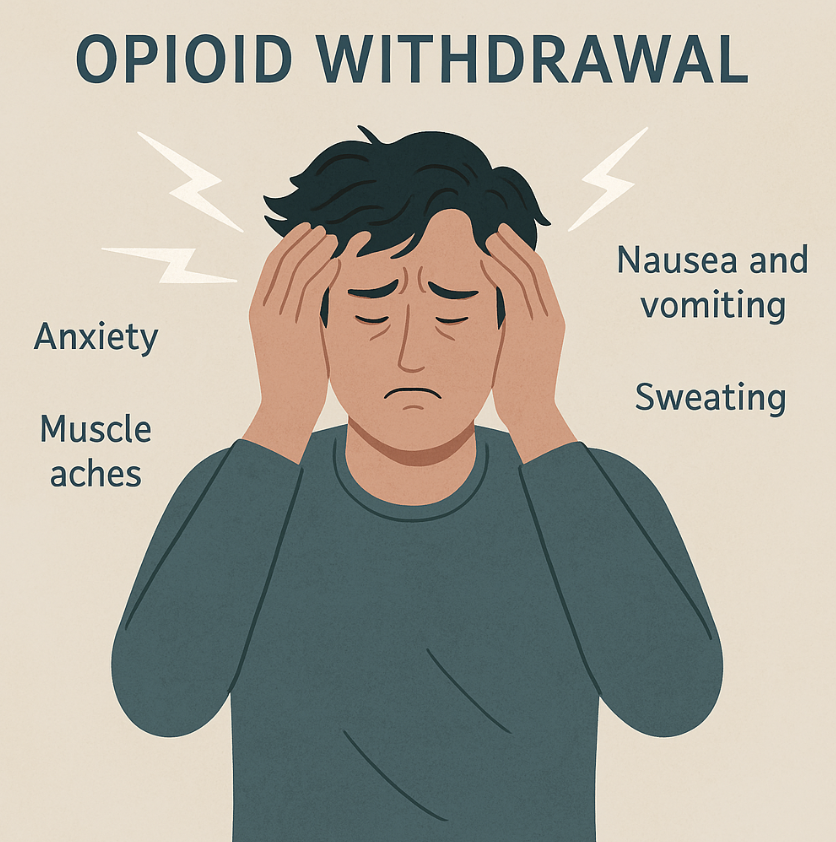
Many describe opioid withdrawal as one of the toughest experiences to endure. The early symptoms typically begin within 6 to 24 hours after the last dose, depending on the opioid used and the individual’s level of dependence. Initial signs such as muscle aches, anxiety, restlessness, and insomnia reflect both physical and psychological distress. The central nervous system, previously subdued by opioids, reacts dramatically to their sudden absence, causing these symptoms.
For many, the psychological impact can be as daunting as the physical. Anxiety, agitation, and mood swings are common, driven by the brain’s struggle to regain balance. Physically, the body exhibits signs like sweating, yawning, and a runny nose, which might seem mild at first but can quickly escalate. These early symptoms serve as a forewarning of the more intense phases of withdrawal, especially in cases involving suboxone withdrawal, that lie ahead.
Opioid withdrawal symptoms and stages
Opioid withdrawal is a journey marked by a progression of symptoms that vary in intensity and duration. Recognizing these stages helps in preparing for and managing the withdrawal process. Typically, withdrawal symptoms unfold in three distinct stages: early-stage, peak, and late-stage.
Each phase presents unique challenges as the body adapts to the absence of opioids.
Early-stage symptoms (6–24 hours)
The early stage of opioid withdrawal, occurring within the first 6 to 24 hours, is characterized by symptoms that are primarily driven by the central nervous system’s response. Anxiety, muscle aches, restlessness, and insomnia are common initial symptoms. Without the opioid’s calming effect, the body enters a hyperactive state, causing agitation and sweating. Though uncomfortable, these symptoms signal the onset of withdrawal.
During this phase, patients may also experience yawning, runny nose, and excessive tearing, often mistaken for flu-like symptoms. These clinical manifestations are the body’s attempt to recalibrate without opioids. While these symptoms can be distressing, they are generally manageable with appropriate care and support.
Peak symptoms (24–72 hours)
The peak stage of withdrawal, occurring between 24 to 72 hours, is often described as the most intense and challenging phase. During this period, withdrawal symptoms peak, causing significant physical discomfort. Common symptoms include severe abdominal cramps, vomiting, and diarrhea. These gastrointestinal issues are particularly debilitating and require careful management to prevent complications like dehydration.
In addition to gastrointestinal distress, patients frequently experience increased heart rate, elevated blood pressure, tachycardia, and restlessness. These indicate an overstimulated nervous system struggling without opioids. Intense cravings during this phase add psychological strain, necessitating medical supervision to prevent relapse.
Late symptoms (3–7+ days)
As withdrawal progresses into the late stage, typically from day 3 onwards, the intensity of physical symptoms begins to wane, but psychological symptoms may persist. Depression, insomnia, and ongoing cravings are common during this phase. Such symptoms can persist for weeks or even months, highlighting the long-term impact of opioid dependence.
The prolonged nature of these symptoms can lead to a condition known as protracted withdrawal, where individuals continue to experience significant withdrawal symptoms long after the acute phase has ended. This stage requires continued support and, often, ongoing medical treatment to ensure a successful recovery.
How long does opioid withdrawal last?
The opiate withdrawal symptoms timeline varies depending on several factors, including the type of opioid used and the individual’s level of dependence. Short-acting opioids like heroin typically lead to withdrawal symptoms that begin within 6 to 12 hours after the last dose and can last for 5 to 7 days. In contrast, long-acting opioids like methadone have a more prolonged onset, with symptoms starting 2 to 4 days after the last dose and potentially lasting for several weeks.
Knowing this timeline aids in preparing for withdrawal. Medically supervised withdrawal offers a structured environment to manage symptoms and minimize complications, ensuring a safer, more effective process.
What makes opioid withdrawal dangerous?
Opioid withdrawal is not only uncomfortable but can also pose significant health risks. Medical complications such as dehydration, due to severe vomiting and diarrhea, can quickly become life-threatening if not properly managed. Additionally, the psychological impacts, including severe anxiety, depression, and suicidal ideation, highlight the need for professional support during withdrawal.
Medically supervised opioid withdrawal is essential as it provides a controlled environment for healthcare professionals to monitor and manage symptoms, reducing complications. This supervision is especially vital for opioid-dependent patients with underlying health conditions that could worsen withdrawal symptoms.
Opioid withdrawal treatment options
There are several effective treatment options for managing opioid withdrawal, ranging from medication-assisted treatment (MAT) to supportive care and detox methods. These treatments seek to alleviate symptoms, prevent complications, and support long-term recovery.
Medication-assisted treatment (MAT)
Medication-assisted treatment (MAT) is a well-recognized and effective strategy for managing opioid addiction treatment. It employs FDA-approved medications such as:
- Methadone: a full opioid agonist that helps stabilize the patient’s condition, allowing for a safer withdrawal process.
- Buprenorphine: a partial agonist that also helps stabilize the patient’s condition for safer withdrawal.
- Naltrexone: used to reduce withdrawal symptoms and cravings.
These medications reduce withdrawal symptoms and cravings, aiding in the management of opioid use disorder.
Naltrexone, an opioid antagonist similar to naloxone, helps prevent relapse by blocking opioids’ euphoric effects. MAT is often combined with counseling and behavioral therapies, providing a holistic approach to treating opioid dependence. Regular monitoring and dosage adjustments are crucial to ensure the effectiveness and safety of these treatments.
Supportive care and detox
Supportive care during detox focuses on managing symptoms to ensure comfort and safety. This care can occur in either inpatient or outpatient settings, based on withdrawal severity and individual needs. Hydration, nutrition, and emotional support are crucial components that enhance detoxification.
Inpatient settings provide continuous medical supervision, crucial for managing severe symptoms and preventing complications. Patient outpatient settings, though less intensive, provide flexibility, allowing patients to maintain daily routines.
Both approaches seek to reduce anxiety and improve overall health during withdrawal.
Home remedies vs. professional help: What’s more effective?
While home remedies may offer temporary relief for mild withdrawal symptoms, they often lack the effectiveness and safety of professional medical treatments. Hydration, exercise, and supplements can help manage some symptoms, but they do not address the underlying issues of opioid dependence.
Professional treatments, like medication-assisted therapy, significantly reduce withdrawal severity and support long-term recovery through pharmacotherapy. For severe symptoms, professional help is vital to ensure safety and efficacy.
Combining home remedies with professional care offers a more comprehensive approach to managing symptoms and prescription medicines.
Post-acute withdrawal syndrome (PAWS)
Post-acute withdrawal syndrome (PAWS) is a condition that can last for weeks or even months after the initial detox phase. PAWS symptoms like anxiety, sleep disturbances, and irritability can significantly impact daily life. These prolonged symptoms highlight the challenges of recovering from opioid addiction, emphasizing the need for ongoing support and treatment.
Managing PAWS often requires a combination of medication, counseling, and lifestyle changes. Addressing these symptoms helps individuals maintain recovery and improve overall quality of life.
When to seek medical help for opioid withdrawal
Knowing when to seek medical help during opioid withdrawal is critical. Red flag symptoms such as hallucinations, severe heart irregularities, or extreme dehydration require immediate medical attention. Medically supervised detox is advised for those with severe dependence to ensure safety and well-being.
Professional help mitigates withdrawal risks and provides access to comprehensive treatments supporting long-term recovery, including a strong support system. Understanding these benefits, implications, and decision points can make a significant difference in the withdrawal process and overall prognosis, reducing risk through assessment.
Bottom Line: Opioid Withdrawal
Opioid withdrawal is a complex and challenging process that requires a comprehensive understanding and approach to manage effectively. From the early symptoms to the late stages and post-acute withdrawal syndrome (PAWS), each phase presents unique challenges that need to be addressed with appropriate treatment and support.
Summarizing the key points, it is evident that medically supervised opioid withdrawal and professional treatments are crucial for ensuring safety and efficacy. By understanding the symptoms, stages, and treatment options, individuals can navigate the withdrawal process more effectively and move towards a life free from opioid dependence. Let’s continue to support each other in this journey towards recovery and well-being.
FAQs about Opioid Withdrawal
Can you die from opioid withdrawal?
Opioid withdrawal is generally not fatal, but it can lead to serious complications such as severe dehydration and suicidal thoughts. Therefore, it is crucial to undergo medically supervised withdrawal to mitigate these risks.
Does everyone experience the same symptoms?
No, individuals do not experience the same symptoms, as the intensity and duration of withdrawal symptoms can vary significantly based on factors such as the type of opioid used and the level of dependence.
Is opioid withdrawal different from other drugs?
Opioid withdrawal is indeed different from that of other drugs, characterized by unique symptoms and a specific progression that necessitates tailored treatments. This distinct nature emphasizes the importance of specialized approaches to manage the withdrawal effectively.
Can withdrawal symptoms return after stopping opioids?
Withdrawal symptoms can indeed return after stopping opioids, often manifesting as post-acute withdrawal syndrome (PAWS), which may include lingering anxiety and insomnia for weeks or even months post-detox.
What treatments are available to ease withdrawal symptoms?
Medication-assisted treatment (MAT) using methadone, buprenorphine, and naltrexone, along with supportive care, can effectively alleviate withdrawal symptoms and aid in recovery.















