Suboxone, combining buprenorphine and naloxone, treats opioid addiction. Buprenorphine eases withdrawal symptoms and cravings, while naloxone prevents misuse. In this article, we will explore Suboxone: how it works and how these components work together to manage addiction.
Key Takeaways
- Suboxone is a combination medication of buprenorphine and naloxone, designed to treat opioid addiction by alleviating withdrawal symptoms and reducing cravings without causing euphoria.
- Suboxone’s mechanism includes buprenorphine’s partial agonist properties, which stabilize brain chemistry, and naloxone’s role in preventing potential misuse, contributing to its effectiveness in Medication-Assisted Treatment.
- It requires careful administration under medical supervision, involves multiple treatment phases, and is more accessible than other MAT options, making it a powerful tool in supporting long-term recovery from opioid use disorder.
What is Suboxone?
Suboxone is a combination medication that consists of buprenorphine and naloxone, designed specifically to treat opioid addiction and opioid dependence. Approved by the FDA for the treatment of opioid use disorder (OUD), this medication has transformed the landscape of addiction treatment by addressing both the physical and psychological aspects of opioid dependence.
Buprenorphine, a partial opioid agonist, binds to the same receptors in the brain as other opioids but activates them less intensely. This helps alleviate withdrawal symptoms and reduce cravings without producing the euphoric high associated with full agonist opioids like heroin or methadone. Naloxone, an opioid antagonist, is included in Suboxone to prevent misuse. If Suboxone is misused by injection, naloxone will block the effects of opioid drugs, precipitating withdrawal and making misuse less appealing. Short-acting opioids and opioid antagonists are crucial in this context for their role in preventing the misuse of opioids.
Suboxone’s unique formulation not only helps manage withdrawal symptoms but also curbs the potential for misuse, making it a safer option for many individuals struggling with opioid drug dependence. This dual action makes Suboxone an essential tool in the fight against opioid addiction, providing a balanced approach to treatment that addresses both immediate and long-term needs.
In essence, Suboxone is more than just a medication; it represents a comprehensive approach to treating opioid addiction. Combining the benefits of buprenorphine and naloxone, Suboxone provides a robust solution for overcoming opioid dependence and reclaiming lives.

Suboxone mechanism of action: How does Suboxone work in the body?
Suboxone’s mechanism of action revolves around its two key components: buprenorphine and naloxone.
Buprenorphine:
- A partial opioid agonist
- Binds to the same receptors in the brain as opioids
- Activates these receptors to a much lesser degree
- Helps alleviate withdrawal symptoms and cravings
- Does not cause the intense euphoria or respiratory depression typical of full opioid agonists
Buprenorphine also has a high affinity for opioid receptors, meaning it binds more strongly than other opioids, effectively blocking them from attaching to these receptors. This unique property minimizes the potential for abuse of additional opioids and reduces the risk of overdose by creating a “ceiling effect”—beyond a certain dose, taking more does not increase its effects.
Naloxone, the other crucial component, acts as an opioid antagonist and is included in Suboxone primarily to deter misuse:
- When taken as prescribed, naloxone is minimally absorbed.
- If someone attempts to misuse Suboxone by injecting it, naloxone will block the effects of opioids.
- This blockage precipitates immediate withdrawal and discourages such behavior.
This combination of buprenorphine and naloxone thus creates a balanced approach to reducing cravings and preventing misuse.
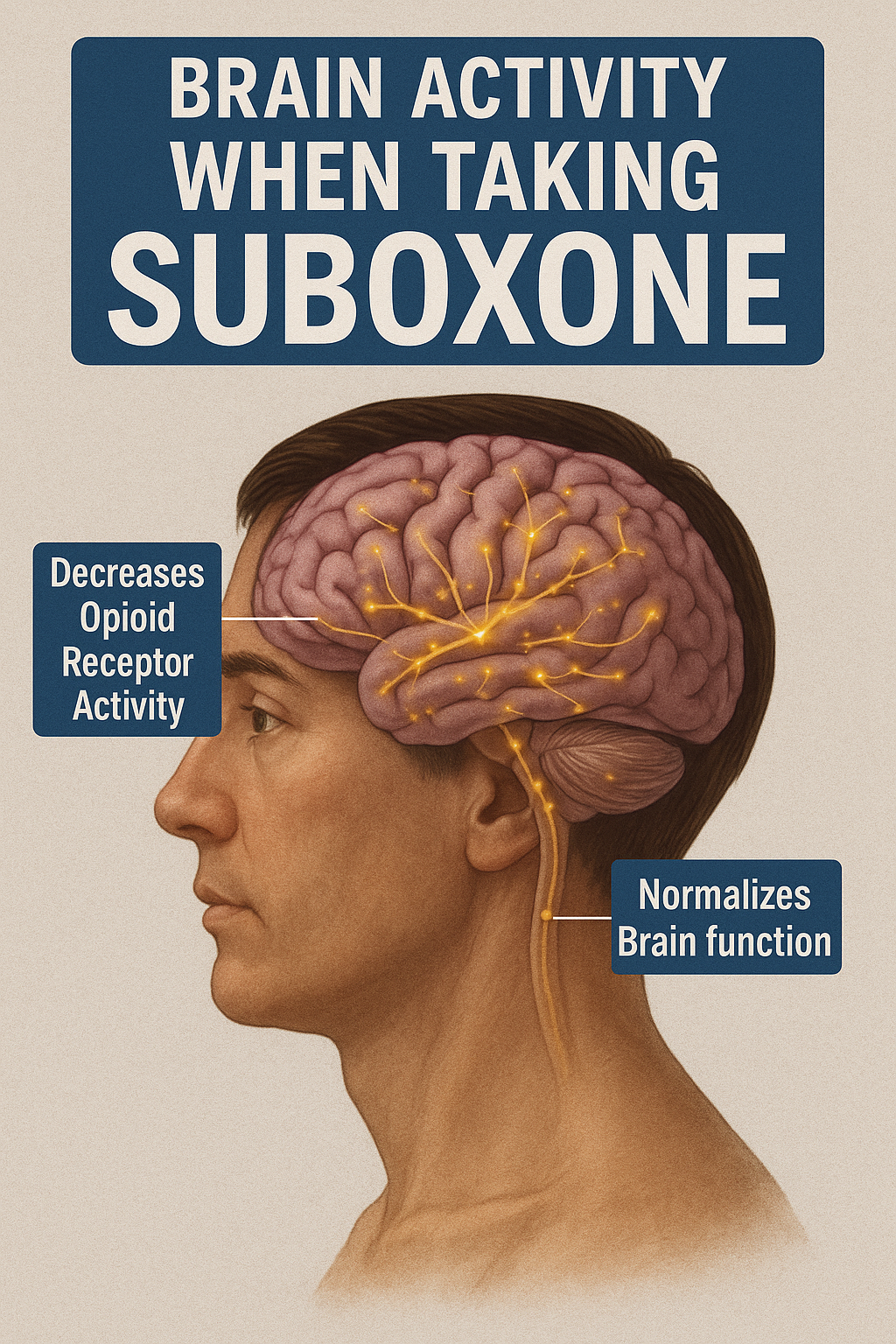
Suboxone also stabilizes brain chemistry during recovery. Maintaining consistent partial activation at opioid receptors it normalizes brain function and reduces the biochemical imbalance from prolonged opioid use. This stabilization is crucial for supporting long-term recovery and reducing the risk of relapse.
Why is Suboxone effective for opioid addiction treatment?
Suboxone plays a pivotal role in Medication-Assisted Treatment (MAT) for opioid addiction. This approach combines medications with counseling and behavioral therapies to provide a “whole-patient” approach to treatment. Suboxone, by reducing withdrawal symptoms and opioid cravings, addresses two of the most significant barriers to overcoming opioid addiction.
Clinical studies have shown that Suboxone is effective in reducing relapse rates and improving retention in treatment programs. The buprenorphine component provides enough receptor activation to minimize withdrawal discomfort without inducing a euphoric high. This helps individuals maintain their treatment regimen and reduces the likelihood of relapse.
Compared to other MAT options, such as Suboxone vs methadone, Suboxone offers several advantages:
- Methadone, a full opioid agonist, requires daily visits to a treatment center, which can be a significant barrier for many patients.
- Naltrexone, an opioid antagonist, requires complete detoxification before it can be initiated, which can also be a challenge.
- Suboxone’s long-acting nature allows for home-based treatment, offering flexibility and convenience.
Combining buprenorphine and naloxone, Suboxone addresses withdrawal symptoms and reduces the risk of misuse. This balanced approach makes Suboxone a powerful tool in the fight against opioid addiction, providing a comprehensive solution that supports both the physiological and psychological aspects of recovery.

What happens in the brain when you take Suboxone?
Suboxone’s components, buprenorphine and naloxone, interact with the brain’s mu-opioid receptors. As a partial agonist, buprenorphine binds to these receptors, alleviating pain and withdrawal symptoms without producing the full effects of stronger opioids. This interaction helps in reducing cravings and stabilizing the brain’s chemistry during recovery.
Buprenorphine’s “ceiling effect” is a key feature. Unlike full opioid agonists, its effects plateau at a certain dose. Higher doses do not increase euphoria, significantly lowering the risk of opioid overdose and misuse. Naloxone, included in Suboxone, blocks the effects of other opioids, further preventing overdose by displacing opioids from their receptors.
Over time, Suboxone normalizes brain function by alleviating the biochemical imbalance from prolonged opioid use. This stabilization is crucial for long-term recovery as it impacts neurotransmitter activity, including dopamine modulation, which affects mood and reward pathways. By addressing these aspects, Suboxone helps individuals regain control over their lives and supports a more stable and rewarding recovery process.
When and how is Suboxone administered?
Suboxone is commonly administered in the form of sublingual tablets or films. Before using a sublingual film, follow these steps:
- Moisten the mouth with water to help the film dissolve effectively.
- Place the film under the tongue.
- Leave the film until it completely dissolves, without chewing or swallowing.
This method ensures that the medication is absorbed directly into the bloodstream, providing quick and effective relief from withdrawal symptoms in medicine.
Key guidelines for Suboxone dosing include:
- Initial doses should begin only when moderate withdrawal signs are evident.
- The first dose should be at least six hours after the last opioid use to avoid Suboxone withdrawal.
- During the maintenance dose phase, the dosage may be adjusted to effectively suppress withdrawal symptoms and cravings.
Suboxone must be taken exactly as prescribed by a healthcare provider. Following the doctor’s instructions on the medication label ensures safe and effective treatment. Suboxone should not be crushed or broken for inhalation or injection, as this can lead to severe health risks and even death.
Healthcare providers, including DATA-waivered providers and nurse practitioners, can prescribe buprenorphine. Patients should inform healthcare professionals about their Suboxone treatment to ensure coordinated care and manage potential emergencies. This collaborative approach optimizes treatment outcomes and supports long-term recovery.
How long does Suboxone stay in your system?
The effects of Suboxone are long-lasting, which supports once-daily dosing. Key points include:
- Buprenorphine, the partial opioid agonist in Suboxone, has a half-life of 24 to 42 hours.
- Naloxone, the opioid antagonist, has a half-life of 2 to 12 hours.
- This prolonged action helps maintain stable levels of the medication in the body.
- It reduces the frequency of dosing and supports a more manageable treatment regimen.
Knowing how long Suboxone stays in your system is important for drug testing, metabolism, and tapering plans. The long half-life of buprenorphine means it can be detected in the body for several days after the last dose, which is crucial for monitoring compliance and planning tapering strategies.
Effective tapering plans ensure a gradual reduction in dosage, minimizing withdrawal symptoms and supporting a smoother transition to long-term sobriety.
What are the side effects and risks of Suboxone?
Like any medication, Suboxone comes with potential side effects. Common side effects include:
- headache
- constipation
- nausea
- sweating
These symptoms are generally mild and tend to diminish as the body adjusts to the medication. However, it’s essential to monitor these side effects and communicate with a healthcare provider to ensure they do not interfere with treatment.
There are also serious risks associated with Suboxone, particularly if it is combined with other sedatives or used improperly. Respiratory depression is a significant risk if Suboxone is mixed with sedatives or alcohol. Additionally, long-term use of Suboxone requires regular monitoring to avoid liver issues and ensure the medication remains effective.
Naloxone, included in Suboxone, can precipitate opioid withdrawal if used too early during detox. This reaction occurs because naloxone displaces opioids from their receptors, leading to immediate opioid withdrawal symptoms. Following the prescribed timing and dosage avoids this uncomfortable and potentially harmful effect.
Long-term use of Suboxone is generally considered safe with proper medical supervision. Key aspects include:
- Regular check-ins with a healthcare provider to monitor any adverse effects
- Adjusting the treatment plan as needed
- Ongoing support to manage side effects and ensure long-term treatment effectiveness.
Who should or shouldn’t take Suboxone?
Suboxone is highly effective for individuals with moderate-to-severe opioid use disorder (OUD) and substance use disorder. These patients often struggle with intense cravings and withdrawal symptoms that can derail their recovery efforts. Suboxone’s ability to reduce these symptoms makes it ideal for such individuals, supporting their journey toward long-term sobriety.
However, Suboxone is not suitable for everyone. Contraindications include severe respiratory issues, certain liver conditions, and known allergies to buprenorphine or naloxone. Additionally, individuals with a history of severe substance use disorders involving multiple drugs may require a more intensive treatment plan that includes other MAT options or inpatient care.
Populations such as pregnant individuals, adolescents, and people with liver conditions should approach Suboxone treatment with caution:
- Pregnant individuals need to weigh the benefits and risks carefully, often in consultation with a specialist.
- Adolescents may need tailored treatment plans considering their developmental needs.
- Those with liver conditions require close monitoring to avoid complications.
Can Suboxone be addictive or misused?
While Suboxone has a lower risk of misuse compared to full opioid agonists, it is not entirely free from the potential for dependency. Buprenorphine, the partial opioid agonist in Suboxone, can lead to physical dependence, especially if used over a long period. However, this dependence is generally manageable under medical supervision and does not equate to addiction, which involves compulsive use despite harmful consequences.
Naloxone discourages misuse of Suboxone in the following ways:
- If the medication is injected, naloxone will precipitate withdrawal symptoms.
- These withdrawal symptoms make misuse less appealing.
- This feature significantly reduces the likelihood of Suboxone being misused via injection, which is a common route for opioid abuse.
Differentiating between physical dependence and addiction is important. Physical dependence is a physiological state where the body adapts to the presence of a drug, leading to withdrawal symptoms if the drug is abruptly discontinued. Addiction, on the other hand, involves psychological cravings and compulsive behavior. Suboxone manages physical dependence while reducing the risk of developing an addiction.
How does Suboxone compare to other MAT options?
Comparing Suboxone to other medications in Medication-Assisted Treatment (MAT) options like methadone and naltrexone involves several factors. Suboxone combines buprenorphine, a partial opioid agonist, with naloxone, an opioid antagonist, which helps prevent misuse. This combination provides a balanced approach to treatment.
Suboxone is known for its ceiling effect, meaning that higher doses do not result in increased euphoria, thereby lowering overdose risks. This makes it a safer option compared to methadone. Key differences include:
- Suboxone has a ceiling effect, while methadone is a full opioid agonist with no ceiling effect, posing a higher risk of overdose.
- Suboxone can be prescribed in various settings, enhancing accessibility.
- Methadone often requires daily visits to a treatment center.
Suboxone treatment’s flexibility accommodates patients who prefer to integrate treatment options into their daily lives. Methadone may be more suitable for individuals with severe opioid dependence due to its stronger effects.
Naltrexone, an opioid antagonist, requires complete detoxification before initiation, posing a challenge for many patients. Each MAT option has benefits and limitations; the choice depends on the patient’s lifestyle, risk profile, and access to clinics.
How is Suboxone used in a complete addiction recovery plan?
Suboxone is integrated into a comprehensive treatment strategy that includes medications, counseling, and behavioral therapy, along with behavioral interventions for managing opioid use disorder (OUD). This holistic approach addresses addiction’s multifaceted nature, supporting both the physical and psychological aspects of recovery.
Suboxone therapy generally consists of three phases:
- Induction: The goal is to safely transition the patient from opioids to Suboxone, minimizing withdrawal symptoms.
- Stabilization: This withdrawal phase involves adjusting the dose to ensure the patient remains comfortable and free of cravings.
- Maintenance: Focuses on long-term treatment, helping patients sustain their recovery.
Regular follow-ups and dose adjustments are crucial components of Suboxone treatment. Check-ins with healthcare providers help monitor progress, manage side effects, and adjust the treatment plan. Tapering strategies may be considered when the patient is ready to reduce their reliance on Suboxone and transition to a drug-free life.
Addressing co-occurring mental health disorders is vital for enhancing overall recovery. Many individuals with opioid addiction struggle with conditions like depression or anxiety, which can hinder their progress. Integrating mental health services into the treatment plan ensures a comprehensive approach supporting long-term sobriety and overall well-being, particularly for those facing opioid use disorders.
Bottom Line: Is Suboxone the right option for you or your loved one?
Suboxone treatment significantly helps those struggling with opioid addiction by reducing cravings and withdrawal symptoms, contributing to an improved quality of life. It offers a balanced approach that addresses both the physical and psychological aspects of addiction, making it a powerful tool to treat opioid dependence in the journey toward recovery.
Candidates for Suboxone treatment must undergo a thorough evaluation considering their medical history, health goals, and existing health issues. This evaluation ensures that Suboxone is the right fit for their specific needs and circumstances. Consulting with a licensed addiction specialist is crucial for developing a personalized treatment plan that maximizes success.
Accessibility is an important factor in the effectiveness of Suboxone treatment. Many health insurance plans cover Suboxone, and telehealth options have made it more accessible. This increased accessibility ensures that more individuals can benefit from this life-saving medication, paving the way for a healthier, addiction-free future.
FAQs about how Suboxone works
Does Suboxone get you high?
Suboxone does not get you high, as its active ingredient, buprenorphine, only partially activates opioid receptors, thus alleviating cravings and withdrawal symptoms without causing euphoria. This unique property makes it effective in treating opioid addiction without the risk of producing a typical opioid high.
Can you still feel pain on Suboxone?
Yes, you can still feel pain while taking Suboxone, as its partial agonist properties make it less effective for pain relief compared to full agonist opioids. Therefore, additional pain management strategies may be necessary for those with chronic pain.
What happens if you take Suboxone too early?
Taking Suboxone too early can trigger withdrawal symptoms due to naloxone displacing existing opioids from their receptors. It is essential to wait until moderate withdrawal symptoms are present before initiating treatment.
Can Suboxone show up on a drug test?
Suboxone can indeed show up on a drug test due to its active ingredient, buprenorphine, which remains detectable in the body for several days after use. Therefore, if you are prescribed Suboxone, it's important to inform testing personnel beforehand.
How long does Suboxone stay in your system?
Suboxone can remain in your system for several days, with buprenorphine having a half-life of 24 to 42 hours and naloxone between 2 to 12 hours. Consequently, it may be detectable for an extended period following the last dose.